Introduction

Lung disease refers to several types of diseases or disorders that prevent the lungs from functioning properly. Lung disease can affect respiratory function, or the ability to breathe, and pulmonary function, which is how well lungs work.
There are many different lung diseases, some of which are caused by bacterial, viral, or fungal infections. Other lung diseases are associated with environmental factors, including asthma, mesothelioma, and lung cancer.
Chronic lower respiratory diseases is a set of conditions that includes chronic obstructive pulmonary disease (COPD), emphysema, and chronic bronchitis. Together, chronic lower respiratory diseases are a leading cause of death in the United States.1
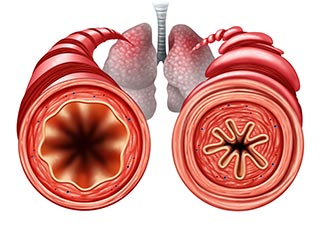
Respiratory diseases such as asthma and COPD involve a narrowing or blockage of airways that reduce air flow.
In other lung conditions ̶ such as pulmonary fibrosis, a lung tissue scarring that can be caused by different factors, and pneumonia, a bacterial or viral infection in which air sacs fill with fluid ̶ the lungs have reduced ability to hold air.
Lung cancer is a disease caused by the abnormal growth of cells. Though most lung cancer starts in the lungs, some cases start in other parts of the body and spread to the lungs. The two main types of lung cancer—small cell and non-small cell—grow and spread in different ways, and each type may be treated differently.
Cigarette smoking is the overall leading cause of lung cancer. Breathing secondhand smoke can also increase a person’s chance of developing the disease.
Other environmental factors linked to lung disease include asbestos, radon gas, air pollution, and chemicals such as uranium, beryllium, vinyl chloride, and arsenic.2
-
Health, United States, 2015. U.S. Department of Health and Human Services. Centers for Disease Control and Prevention. National Center for Health Statistics. [DHHS Publication 2016-1232 Health, United States, 2015. U.S. Department of Health and Human Services. Centers for Disease Control and Prevention. National Center for Health Statistics.]
-
Reid PT, Innes JA. Respiratory disease. In: Walker BR, Colledge NR, Ralston SH, Penman ID, eds. Davidson’s Principles and Practice of Medicine. 22nd ed. Philadelphia, PA: Elsevier Churchill Livingstone; 2014:chap 19.
What is NIEHS Doing?
NIEHS conducts and funds studies to understand the genetic and environmental contributions to lung disease development, and to identify new ways to prevent and treat lung disease in people.
Air pollution studies – Long-term exposure to air pollutants can affect lung development and increase the chance of developing asthma, emphysema, and other respiratory diseases. Results from the NIEHS-supported Harvard Six Cities Study, the largest available database on the health effects of outdoor and indoor air pollution, show a strong association between exposure to ozone, fine particles, and sulfur dioxide with an increase in breathing problems, reduced lung capacity, and risk of early death.
Lung-on-a-chip – NIEHS supported development of a three-dimensional model of a breathing human lung on a microchip.3 This model tests the effects of environmental exposures, as well as the safety of new drugs.
Genetics and lung function – By analyzing data from studies around the world, NIEHS researchers and their collaborators identified more than 50 genetic changes that affect the risk of pulmonary disorders in people of European, African, Asian, and Hispanic descent.4 Several of these changes could affect how some drugs are developed to treat lung function problems.
Risk of respiratory disease – Mutations in a gene called macrophage receptor with collagenous structure, or MARCO, contributed to the severity of respiratory syncytial virus (RSV) disease in infants.5 The findings may help identify people who have a greater chance of developing severe RSV infection and provide treatments to prevent disease.
Hexavalent chromium and lung changes – Drinking water contaminated with hexavalent chromium, an industrial chemical, can lead to genetic changes in human lung cells. These changes included permanent alterations in DNA molecules that carry genetic information, known as chromosomes, as well as problems in DNA repair.6
Air pollution and COPD – Breathing air pollution can lead to COPD, as shown by a NIEHS-funded study that found diesel exhaust particles, a major source of air pollution, dampened the activity of genes involved stress response in the lung.7
Lung cancer treatment – Non−small-cell lung cancer is often resistant to chemotherapy. Related to this type of cancer, NIEHS researchers found that silencing a gene called INO80 led to reduced tumor growth, potentially leading to better treatment options and improved patient outcomes.8
Mold exposure and lung disease – Mice that inhaled spores from the mold Aspergillus fumigatus, which is typical of moisture-damaged buildings, developed allergic and inflammatory reactions when the mold spores sprouted new growth.9 ,10 The findings may influence the development of treatments for respiratory illnesses associated with mold exposure.
New biomarker for a respiratory condition – NIEHS researchers and their collaborators identified cholestenoic acid as a novel biomarker, a measurable substance in the body that indicates disease, for acute respiratory distress syndrome (ARDS), a life-threatening respiratory condition characterized by tissue damage and fluid buildup in the lungs. ARDS is deadly in 30-40% of cases, and only a few lung biomarkers have been validated.11
Ambient air pollution and asthma – Two large NIEHS-funded studies show an association between decreases in levels of air pollutants and improvements in lung function along with reductions in asthma symptoms.12 ,13 The findings underscore the importance of air pollution reduction policies and strategies on improved air quality and health.
NIEHS-funded, large-scale studies
- E-Cigs and Smoking – This study is developing new biomarkers, measurable substances in the body that indicate disease, of tobacco smoke exposure or e-cigarette use.
- Gulf Long-term Follow Up Study (GuLF) – This study looks at health effects in workers and volunteers who helped with the oil spill response and clean-up following the Deepwater Horizon disaster.
- Natural History of Asthma with Longitudinal Environmental Sampling (NHALES) – This study seeks understanding of how bacteria and other factors in the environment affect people who have moderate to severe asthma.
-
Huh D, Matthews BD, Mammoto A, Montoya-Zavala M, Hsin HY, Ingber DE. Reconstituting organ-level lung functions on a chip. Science 328(5986):1662-1668. [Abstract Huh D, Matthews BD, Mammoto A, Montoya-Zavala M, Hsin HY, Ingber DE. Reconstituting organ-level lung functions on a chip. Science 328(5986):1662-1668.]
-
Wyss AB, Sofer T, Lee MK, Terzikhan N, Nguyen JN, Lahousse L, Latourelle JC, Smith AV, Bartz TM, Feitosa MF, Gao W, Ahluwalia TS, Tang W, Oldmeadow C, Duan Q, de Jong K, Wojczynski MK, Wang XQ, Noordam R, Hartwig FP, Jackson VE, Wang T, M Obeidat M, Hobbs BD, Huan T, Gui H, Parker MM, Hu D, Mogil LS, Kichaev G, Jin J, Graff M, Harris TB, Kalhan R, Heckbert SR, Paternoster L, Burkart KM, Liu Y, Holliday EG, Wilson JG, Vonk JM, Sanders JL, Barr RG, de Mutsert R, Menezes AMB, Adams HHH, van den Berge M, Joehanes R, Levin AM, Liberto J, Launer LJ, Morrison AC, Sitlani CM, Celedon JC, Kritchevsky SB, Scott RJ, Christensen K, Rotter JI, Bonten TN, Wehrmeister FC, Bosse Y, Xiao S, Oh S, Franceschini N, Brody JA, Kaplan RC, Lohman K, McEvoy M, Province MA, Rosendaal FR, Taylor KD, Nickle DC, Williams LK, Burchard EG, Wheeler HE, Sin DD, Gudnason V, North KE, Fornage M, Psaty BM, Myers RH, OâConnor G, Hansen T, Laurie CC, Cassano PA, Sung J, Kim WJ, Attia JR, Lange L, Boezen HM, Thyagarajan B, Rich SS, Mook-Kanamori DO, Horta BL, Uitterlinden AG, Im HK, Cho MH, Brusselle GG, Gharib SA, Dupuis J, Manichaikul A, London SJ. 2018. Multiethnic meta-analysis identifies ancestry-specific and cross-ancestry loci for pulmonary function. Nat Commun 9(1):2976. [Abstract Wyss AB, Sofer T, Lee MK, Terzikhan N, Nguyen JN, Lahousse L, Latourelle JC, Smith AV, Bartz TM, Feitosa MF, Gao W, Ahluwalia TS, Tang W, Oldmeadow C, Duan Q, de Jong K, Wojczynski MK, Wang XQ, Noordam R, Hartwig FP, Jackson VE, Wang T, M Obeidat M, Hobbs BD, Huan T, Gui H, Parker MM, Hu D, Mogil LS, Kichaev G, Jin J, Graff M, Harris TB, Kalhan R, Heckbert SR, Paternoster L, Burkart KM, Liu Y, Holliday EG, Wilson JG, Vonk JM, Sanders JL, Barr RG, de Mutsert R, Menezes AMB, Adams HHH, van den Berge M, Joehanes R, Levin AM, Liberto J, Launer LJ, Morrison AC, Sitlani CM, Celedon JC, Kritchevsky SB, Scott RJ, Christensen K, Rotter JI, Bonten TN, Wehrmeister FC, Bosse Y, Xiao S, Oh S, Franceschini N, Brody JA, Kaplan RC, Lohman K, McEvoy M, Province MA, Rosendaal FR, Taylor KD, Nickle DC, Williams LK, Burchard EG, Wheeler HE, Sin DD, Gudnason V, North KE, Fornage M, Psaty BM, Myers RH, OâConnor G, Hansen T, Laurie CC, Cassano PA, Sung J, Kim WJ, Attia JR, Lange L, Boezen HM, Thyagarajan B, Rich SS, Mook-Kanamori DO, Horta BL, Uitterlinden AG, Im HK, Cho MH, Brusselle GG, Gharib SA, Dupuis J, Manichaikul A, London SJ. 2018. Multiethnic meta-analysis identifies ancestry-specific and cross-ancestry loci for pulmonary function. Nat Commun 9(1):2976.]
-
High M, Cho HY, Marzec J, Wiltshire T, Verhein KC, Caballero MT, Acosta PL, Ciencewicki J, McCaw ZR, Kobzik L, Miller-DeGraff L, Gladwell W, Peden DB, Serra ME, Shi M, Weinberg C, Suzuki O, Wang X, Bell DA, Polack FP, Kleeberger SR. 2016. Determinants of host susceptibility to murine respiratory syncytial virus (RSV) disease identify a role for the innate immunity scavenger receptor MARCO gene in human infants. EBioMedicine 11:73â84. doi: 10.1016/j.ebiom.2016.08.011. [Online 6 Aug 2016]. [Abstract High M, Cho HY, Marzec J, Wiltshire T, Verhein KC, Caballero MT, Acosta PL, Ciencewicki J, McCaw ZR, Kobzik L, Miller-DeGraff L, Gladwell W, Peden DB, Serra ME, Shi M, Weinberg C, Suzuki O, Wang X, Bell DA, Polack FP, Kleeberger SR. 2016. Determinants of host susceptibility to murine respiratory syncytial virus (RSV) disease identify a role for the innate immunity scavenger receptor MARCO gene in human infants. EBioMedicine 11:73â84. doi: 10.1016/j.ebiom.2016.08.011. [Online 6 Aug 2016].]
-
Wise SS, Aboueissa AE, Martino J, Wise JP Sr. 2018. Hexavalent chromium-induced chromosome instability drives permanent and heritable numerical and structural changes and a DNA repair-deficient phenotype. Cancer Res 78(15):4203â4214. [Abstract Wise SS, Aboueissa AE, Martino J, Wise JP Sr. 2018. Hexavalent chromium-induced chromosome instability drives permanent and heritable numerical and structural changes and a DNA repair-deficient phenotype. Cancer Res 78(15):4203â4214.]
-
Li X, Yang H, Sun H, Lu R, Zhang C, Gao N, Meng Q, Wu S, Wang S, Aschner M, Wu J, Tang B, Gu A, Kay SA, Chen R. 2017. Taurine ameliorates particulate matter-induced emphysema by switching on mitochondrial NADH dehydrogenase genes. Proc Natl Acad Sci U S A 114(45):E9655âE9664. [Abstract Li X, Yang H, Sun H, Lu R, Zhang C, Gao N, Meng Q, Wu S, Wang S, Aschner M, Wu J, Tang B, Gu A, Kay SA, Chen R. 2017. Taurine ameliorates particulate matter-induced emphysema by switching on mitochondrial NADH dehydrogenase genes. Proc Natl Acad Sci U S A 114(45):E9655âE9664.]
-
Zhang S, Zhou B, Wang L, Li P, Bennett BD, Snyder R, Garantziotis S, Fargo DC, Cox AD, Chen L, Hu G. 2017. INO80 is required for oncogenic transcription and tumor growth in non-small cell lung cancer. Oncogene 36(10):1430-1439. [Abstract Zhang S, Zhou B, Wang L, Li P, Bennett BD, Snyder R, Garantziotis S, Fargo DC, Cox AD, Chen L, Hu G. 2017. INO80 is required for oncogenic transcription and tumor growth in non-small cell lung cancer. Oncogene 36(10):1430-1439.]
-
Nayak AP, Green BJ, Lemons AR, Marshall NB, Goldsmith WT, Kashon ML, Anderson SE, Germolec DR, Beezhold DH. 2016. Subchronic exposures to fungal bioaerosols promotes allergic pulmonary inflammation in naive mice. Clin Exp Allergy 46(6):861-70. [Abstract Nayak AP, Green BJ, Lemons AR, Marshall NB, Goldsmith WT, Kashon ML, Anderson SE, Germolec DR, Beezhold DH. 2016. Subchronic exposures to fungal bioaerosols promotes allergic pulmonary inflammation in naive mice. Clin Exp Allergy 46(6):861-70.]
-
Nayak AP, Croston TL, Lemons AR, Goldsmith WT, Marshall NB, Kashon ML, Germolec DR, Beezhold DH, Green BJ. 2018. Aspergillus fumigatus viability drives allergic responses to inhaled conidia. Ann Allergy Asthma Immunol 121(2):200-210.e2. [Abstract Nayak AP, Croston TL, Lemons AR, Goldsmith WT, Marshall NB, Kashon ML, Germolec DR, Beezhold DH, Green BJ. 2018. Aspergillus fumigatus viability drives allergic responses to inhaled conidia. Ann Allergy Asthma Immunol 121(2):200-210.e2.]
-
Madenspacher JH, Stapleton RD, Suratt BT, Dixon AE, Lih FB, Lowe JM, Mould KJ, Janssen WJ, Morrell ED, Wurfel MM, Garantziotis S, Tomer KB, Fessler MB. 2018. Cholestenoic acid is a prognostic biomarker in acute respiratory distress syndrome. J Allergy Clin Immunol. 143(1):440-442 [Abstract Madenspacher JH, Stapleton RD, Suratt BT, Dixon AE, Lih FB, Lowe JM, Mould KJ, Janssen WJ, Morrell ED, Wurfel MM, Garantziotis S, Tomer KB, Fessler MB. 2018. Cholestenoic acid is a prognostic biomarker in acute respiratory distress syndrome. J Allergy Clin Immunol. 143(1):440-442]
-
Berhane K, Chang CC, McConnell R, Gauderman WJ, Avol E, Rapapport E, Urman R, Lurmann F, Gilliland F. 2016. Association of changes in air quality with bronchitic symptoms in children in California, 1993-2012. JAMA 315(14):1491-1501. [Abstract Berhane K, Chang CC, McConnell R, Gauderman WJ, Avol E, Rapapport E, Urman R, Lurmann F, Gilliland F. 2016. Association of changes in air quality with bronchitic symptoms in children in California, 1993-2012. JAMA 315(14):1491-1501.]
-
Gauderman WJ, Urman R, Avol E, Berhane K, McConnell R, Rappaport E, Chang R, Lurmann F, Gilliland F. 2015. Association of improved air quality with lung development in children. N Engl J Med 372(10):905-913. [Abstract Gauderman WJ, Urman R, Avol E, Berhane K, McConnell R, Rappaport E, Chang R, Lurmann F, Gilliland F. 2015. Association of improved air quality with lung development in children. N Engl J Med 372(10):905-913.]
Further Reading
Stories from the Environmental Factor (NIEHS Newsletter)
- Targeting Mouse Cells, Rather Than Bacteria, to Treat Pneumonia (December 2021)
- Biomarker Suggests Severity of COVID-19 Respiratory Distress (May 2021)
- Environmentally Persistent Free Radicals May Affect Lung Health (May 2021)
- Intense Allergic Asthma Mechanism Discovered in Mice (May 2021)
- Chronic Lung Disease Responds to Hyaluronan in NIEHS-led Study (March 2021)
Fact Sheets
Lung Health and Your Environment
Press Releases
- NIH Study Illuminates Origins of Lung Cancer in Never Smokers (Sept. 6, 2021) – Study insights will help unlock the mystery of how lung cancer arises in people who have never smoked. The results may guide development of more precise clinical treatments. The study was conducted by the Intramural Research Program of the National Cancer Institute and NIEHS.
Additional Resources
- Be Tobacco Free – An U.S. Department of Health and Human Services website that provides tools to help people quit smoking.
- Chronic Obstructive Pulmonary Disease: Learn More Breathe Better – This program offers several educational resources to increase awareness and understanding about lung diseases and conditions.
- 15th Report on Carcinogens – A congressionally mandated, science-based, public health document by the National Toxicology Program that describes agents, substances, mixtures, and exposure circumstances that are likely to cause cancer in humans.



