Introduction

A healthy immune system defends the body against disease and infection. But if the immune system malfunctions, it mistakenly attacks healthy cells, tissues, and organs. Called autoimmune disease, these attacks can affect any part of the body, weakening bodily function and even turning life-threatening.
Scientists know about more than 80 autoimmune diseases. Some are well known, such as type 1 diabetes, multiple sclerosis, lupus, and rheumatoid arthritis, while others are rare and difficult to diagnose. With unusual autoimmune diseases, patients may suffer years before getting a proper diagnosis. Most of these diseases have no cure. Some require lifelong treatment to ease symptoms.
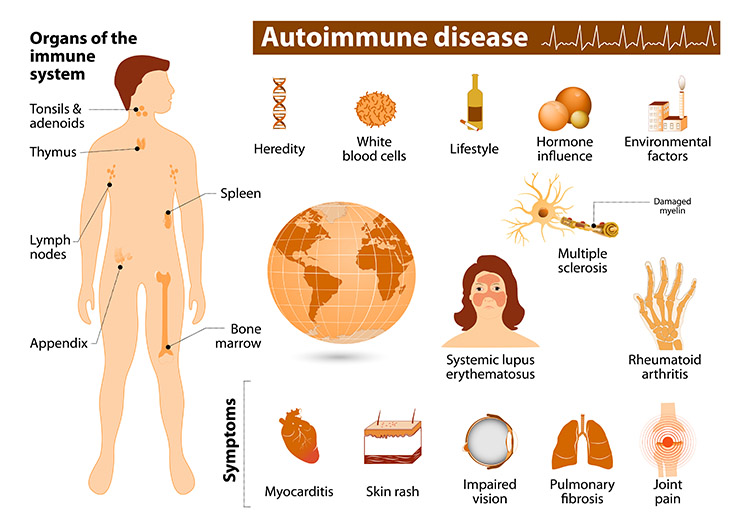
Studies indicate these diseases likely result from interactions between genetic and environmental factors. Sex, race, and ethnicity characteristics are linked to a likelihood of developing an autoimmune disease.1 Autoimmune diseases are more common when people are in contact with certain environmental exposures, as described below.
-
Ramos PS, Shedlock AM, Langefeld, CD. 2015. Genetics of autoimmune diseases: insights from population genetics. J Hum Genet. 60(11): 657â664. [Abstract Ramos PS, Shedlock AM, Langefeld, CD. 2015. Genetics of autoimmune diseases: insights from population genetics. J Hum Genet. 60(11): 657â664.]
What is NIEHS Doing?
Unraveling the genetic and environmental underpinnings of autoimmune disease is a focus at NIEHS and the National Toxicology Program (NTP). Progress happens through multiple research efforts, such as:
- Sunlight associated with autoimmune disease – This NIEHS study suggests exposure to ultraviolet radiation from sunlight may be connected to the development of juvenile dermatomyositis, an autoimmune disease associated with muscle weakness and skin rashes.
- Childhood poverty linked to rheumatoid arthritis in adulthood – NIEHS researchers discovered a link between lower socioeconomic status in childhood and rheumatoid arthritis in adulthood. The effect of lower childhood socioeconomic status and lower adult education level equaled the combined effect of having both a paternal and personal history of smoking.
- Agricultural chemicals and rheumatoid arthritis – Researchers at NIEHS found that exposure to some pesticides may play a role in the development of rheumatoid arthritis in male farm workers.
- Organic mercury may trigger autoimmune disease – In a study funded by NIEHS, methylmercury, even at exposure levels generally considered safe, may be linked to development of autoimmune antibodies in women of reproductive age. These antibodies could lead in turn to autoimmune diseases, such as inflammatory bowel disease, lupus, rheumatoid arthritis, and multiple sclerosis.
- Genetic factors in autoimmune muscle disease – NIEHS researchers identified the primary genetic risk factors associated with autoimmune muscle disease in Caucasian populations in Europe and the United States.
- Gene-environment interaction in rheumatoid arthritis – A study funded by NIEHS pinpointed the mechanics of a gene-environment interaction that could explain why the genetic risk for rheumatoid arthritis is amplified by environmental pollutants like cigarette smoke.
- Role of nutrition in development of autoimmune disease – NIEHS-funded research indicates that vitamin D may be important for preventing immune dysfunction in older populations. Another study funded by NIEHS found that dietary micronutrients could either improve or worsen lupus symptoms.
Further Reading
Stories from the Environmental Factor (NIEHS Newsletter)
- New Conference Breaks Ground on Developing Tools for Data Collection (December 2024)
- NIH Hosts Visit for People With Myositis (October 2024)
- Lupus Arises From Complex Interplay of Genetic and Environmental Factors (July 2024)
- Certain Pesticides May Increase Risk of Inflammatory Bowel Disease (May 2024)
- Lisa Rider Inducted Into Association of American Physicians (May 2024)
- Autoimmune Diseases and Women’s Health Spotlighted During Webinar (February 2022)
- Scientific Journeys: From Basic Researcher to Leader in Autoimmunity (July 2021)
- Autoimmunity Origins May Lie in Defective Mitochondria (March 2021)
Fact Sheets
Autoimmune Diseases and Your Environment
Additional Resources
- Facts About Autoimmune Diseases - from the NIH Office of Women’s Health
- List of Autoimmune Diseases - from the American Autoimmune Related Diseases Association
- Study Offers New Clues to Why Most People with Autoimmune Diseases Are Women (February 2024) - This blog post by the NIH director discusses why as many as four out of every five people affected by autoimmune diseases are women.
Related Health Topics
This content is available to use on your website.
Please visit NIEHS Syndication to get started.


