Superfund Research Program
By Julie Leibach
Highlights
- Research supported by the NIEHS Superfund Research Program (SRP) informed federal regulations on PFAS in drinking water, set by the U.S. Environmental Protection Agency.
- The Centers for Disease Control and Prevention drew on a report developed, in part, by SRP-funded researchers when updating its clinical guidance on PFAS.
- SRP staff and funded investigators provided subject matter expertise to discussions about PFAS research and development.
Overview
The NIEHS Superfund Research Program (SRP) supported research that helped inform the nation’s first legally enforceable limits on PFAS in drinking water. Announced in April 2024 by the U.S. Environmental Protection Agency (EPA), the regulations build on earlier drinking water advisories issued by the EPA that also drew on SRP-funded studies.
Researchers funded by SRP also provided expertise to a 2022 report published by the National Academies of Sciences, Engineering, and Medicine (NASEM) that guides clinicians in evaluating patients for PFAS exposure and addressing associated health effects. In January 2024, the Centers for Disease Control and Prevention (CDC) updated its clinical guidelines for PFAS, citing the NASEM report.
The Problem
Since PFAS production began in the 1940s, these chemicals have been widely used for their oil- or water-resistance, heat tolerance, and low-friction qualities. A 2020 study funded partly by SRP described more than 200 uses for more than 1,400 individual PFAS, noting that nearly all branches of industry and many everyday products rely on the chemicals. For example, PFAS enhance firefighting suppressants, lubricate jet engines, and curb steel corrosion. They also fend off stains on fabric, lend anti-stickiness to cookware, and imbue makeup with durability.
At any point from production to disposal, PFAS can escape into soil, water, and air, according to a review funded by SRP and others. Held together by strong chemical bonds, the chemicals resist natural degradation and can accumulate in ecosystems and organisms. More than an estimated 2,800 U.S. locations have some level of PFAS contamination — in 2019, the EPA documented 180 PFAS-contaminated Superfund sites alone— and nearly all Americans have been exposed to at least one type of PFAS chemical, according to a NASEM report.
Exposure can occur through various routes, such as ingestion and inhalation. Although certain occupational activities — like painting or firefighting — pose a unique risk, people can breathe in PFAS in everyday environments as well, according to an SRP-funded study cited in the NASEM report. Using sheets made of polyethylene, a type of plastic, researchers measured PFAS levels in kindergarten classrooms and several other indoor locations. They found that carpets and dust are major sources of certain PFAS in indoor air.
Researchers are steadily uncovering how PFAS affect health. Growing evidence suggests that PFAS exposure is associated with negative health effects on the immune system, metabolism, and early development, among other biological systems and processes. International and federal agencies have also linked the chemicals to some cancers.
SRP Solutions
SRP-funded researchers have identified ways that PFAS can harm health, providing valuable information that decision makers can use to better protect communities and patients. Their work has informed federal advisories and regulations for PFAS in drinking water, as well as recommendations for clinical care of patients exposed to the chemicals. SRP staff members have also provided expertise to support the government response to health concerns about PFAS.
Reducing Exposure and Improving Remediation
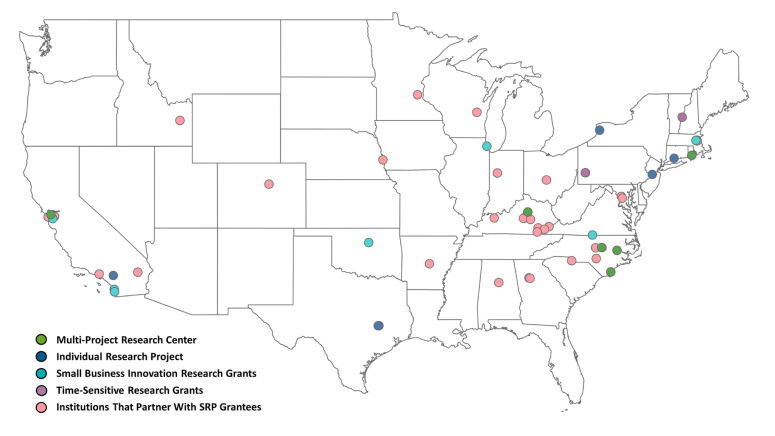
Across the country, SRP-funded researchers are unraveling routes of PFAS exposure and associated health effects. In addition, SRP supports innovative efforts to minimize PFAS exposure and clean up contamination.
For example, a company called CycloPure produces a filter cartridge compatible with popular water pitchers that can remove PFAS from drinking water. The cartridges are based on technology called DEXSORB+, which the company developed through an SRP Small Business Innovation Research Grant.
SRP funding through an individual research grant also enabled investigators with Texas A&M Agrilife Research to develop a plant-based material that adsorbs PFAS, along with microbial fungi that consume the so-called “forever chemicals.”
Working with members of the Mi’kmaq Nation and a community organization in Maine, SRP-funded scientists at Yale University and the Connecticut Agricultural Experiment Station are also using organic material — in this case, hemp plants — to remove PFAS from a contaminated site in the northern part of the state. The team is exploring how treating soil with nanomaterials can enhance PFAS uptake into the plants. (Read this Environmental Factor story.)
Learn more about how SRP grant recipients are discovering new ways to detect and characterize PFAS, remediate the environment from contamination, and communicate potential health risks to communities in the March 2022 Science Digest.
Improving Drinking Water Health Advisories
In 2012, environmental scientist Philippe Grandjean, M.D., D.M.Sc., and colleagues published an NIEHS-funded study showing that high exposures to several PFAS were associated with reduced immune response to tetanus and diphtheria vaccinations in 5- and 7-year-olds from the Faroe Islands.
Grandjean had been following the North Atlantic population since the 1980s, when he started exploring fetal exposure to mercury. As PFAS emerged as a contaminant of concern, his team nimbly reoriented their research focus. Now Grandjean is a project leader with STEEP, for Sources, Transport, Exposure and Effects of PFAS, an SRP Center based at the University of Rhode Island (URI) in partnership with the Harvard John A. Paulson School of Engineering and Applied Sciences and Silent Spring Institute.
In 2018, with SRP funding, Grandjean and University of Denmark colleague Esben Budtz-Jørgensen revealed the level of PFAS exposure necessary to elicit a negative immune response in children like that observed in the earlier study. The researchers focused on perfluorooctanoic acid (PFOA) and perfluorooctane sulfonic acid (PFOS) which, after decades of use, have been predominantly phased out in the U.S.
Both studies were foundational to interim drinking water health advisories for PFOA and PFOS released by the EPA in June 2022. Radhika Fox, of the EPA Office of Water, announced the news at the 3rd National PFAS Meeting, co-funded by NIEHS and organized by a committee that included several SRP grant recipients, among them Grandjean.
“Our findings on PFAS-induced immunotoxicity and our calculations from the SRP-funded study helped EPA determine a reference dose for each contaminant — that is, a concentration level at or below which daily exposure is unlikely to lead to negative health effects,” Grandjean explained.
“The low exposure limits aim to protect all people, including the next generation by limiting the overall intake of PFAS so that new mothers are not passing on toxic amounts through the placenta or via human milk,” he added.
Before publishing the advisories, the EPA considered input from a review panel chaired by Weihsueh Chiu, Ph.D., deputy director of the Texas A&M University (TAMU) SRP Center. Following several public meetings that informed the review, Chiu presented the panel’s recommendations to the EPA in July 2022.
Other SRP grant recipients on the review panel included Oregon State University’s Jamie DeWitt, Ph.D., who is a project leader with the North Carolina State University (NCSU) SRP Center, and Angela Slitt, Ph.D., of the URI SRP Center.
Informing New Drinking Water Regulations
Building on those advisories, in April 2024 the EPA announced the PFAS National Primary Drinking Water Regulation. The final rule sets legally enforceable levels for five individual PFAS in drinking water, including PFOA, PFOS, PFHxS, PFNA, and HFPO-DA. The regulation also sets limits on PFAS mixtures containing at least two or more of the following: PFHxS, PFNA, HFPO-DA, and PFBS. Additionally, the EPA established non-enforceable health-based goals for further reducing PFAS levels in drinking water.
Grandjean and Budtz-Jørgensen’s paper on PFAS and immune response in children informed the new drinking water regulations, as did the following SRP-funded projects:
- Work by Grandjean and colleagues showing that PFAS exposures might interfere with lipid metabolism, which could lead to increased risk for cardiovascular disease.
- A water quality study led by Jennifer Guelfo, Ph.D., formerly a postdoctoral researcher at the previously funded Brown University SRP Center. The team analyzed data from nearly 37,000 drinking water samples collected from almost 5,000 different public water supplies over a two-year period. They detected PFAS in 1.6% of samples, or 4% of the water supplies. Of the samples that contained PFAS, half contained at least two types.
- Research by Yale University SRP Center Director Vasilis Vasiliou, Ph.D., reporting that health outcomes may differ depending on exposure to short-chained versus long-chained PFAS. Short-chained PFAS have fewer carbon-fluorine bonds than long-chained PFAS
Addressing Clinical Gaps
Research and expertise supported by SRP was also key to the NASEM report, announced in July 2022, that provides guidance on testing and clinical care for people exposed to PFAS. To develop recommendations, NASEM appointed a committee whose ranks included several SRP-funded researchers — namely, Melissa Gonzales, Ph.D., of the University of New Mexico SRP Center; Erin Haynes, Ph.D., of the University of Kentucky SRP Center; Jane Hoppin, Ph.D., of the NCSU SRP Center; and Tamarra James-Todd, Ph.D., of the Harvard SRP Center. Former SRP grant recipient Veronica Vieira, D.Sc., of the University of California Irvine, also participated.
Committee members mined the scientific literature for connections between human health effects and PFAS, leaning on several SRP-funded studies to draw conclusions. They focused on the PFAS commonly studied in humans. However, citing a paper co-authored by SRP-funded researchers, they noted that other PFAS with similar biological persistence and toxicities may also be harmful to health.
Among their findings, committee members determined that, based on limited evidence, an association might exist between exposure to PFAS and high blood pressure and preeclampsia in pregnant women. Work published in 2021 by Grandjean and colleagues informed that decision. Although his team found no clear connection between PFAS exposure and high blood pressure or preeclampsia in pregnant women, they did observe slight — albeit, not statistically significant — increases in blood pressure for PFOS and PFOA. Considered at the population level, that association could manifest as an increased incidence of gestational hypertension, the authors explained. High blood pressure during pregnancy could have a lasting effect on the mother’s health and that of her child, they added.
The NASEM committee members also concluded that limited evidence suggests the possibility of a connection between PFAS, thyroid hormones, and thyroid disease. Among several papers, they cited a 2020 study published by Grandjean and team that examined links between PFAS exposure, thyroid hormone levels in pregnant women, and birth outcomes. Overall, the researchers found PFAS to be associated with dysfunction of the thyroid gland.
The committee looked for ties between PFAS and the severity of COVID-19 as well, singling out a study led by Grandjean. After analyzing plasma samples from more than 300 people with COVID-19 for exposure to five types of PFAS, the researchers found that high plasma concentrations of a PFAS chemical called perfluorobutanoic acid were associated with an increased risk of more severe cases of COVID-19.
Because plasma samples indicated an overall low level of exposure to PFAS, however, Grandjean’s team indicated that additional research should explore links between COVID-19 severity and PFAS in populations with higher exposure. For their part, NASEM committee members decided that insufficient evidence exists to conclude how PFAS exposure may influence COVID-19 infection at this time.
Among its recommendations, the NASEM document advises clinicians to offer PFAS blood testing to patients who likely have histories of high exposure, such as workers exposed on the job and people who have either lived in communities with documented contamination or where high exposure may have occurred, such as near commercial airports, military bases, or wastewater treatment plants.
The report also suggests that the CDC, the Agency for Toxic Substances and Disease Registry, and public health departments create educational materials for clinicians to better understand PFAS exposure and potential health effects, as well as the pros, cons, and limitations of testing. To better surveil exposures, laboratories conducting PFAS testing should report the results to state public health authorities, the publication adds.
As they developed the report, committee members sought input from the public through regional town hall meetings and community liaisons, who included Phil Brown, Ph.D., co-director of community engagement efforts at Northeastern University’s SRP Center; DeWitt; Rainer Lohmann, Ph.D., director of the URI SRP Center; and Laurel Schaider, Ph.D., of Silent Spring Institute and the URI SRP Center, among others.
“The goal was to hear the perspectives of people from all around the U.S., including Pacific Islanders and other disproportionately affected communities,” said Brown in a 2021 SRP news story. “This shed light on the similarities across different regions, the issues they are facing, and their concerns.”
The town halls, hosted virtually, included presentations by community representatives about exposures, health effects, and health care needs, as well as discussion sessions between committee members and participants.
“Overwhelmingly, community members want their exposures and potential health risks to be taken seriously,” observed DeWitt in the SRP news story. “They would like to have more information about their exposure levels and how to prevent adverse health effects.”
Before releasing the report, the committee requested a formal review from a panel that included Julia Brody, Ph.D., of Silent Spring Institute and the URI SRP Center, Grandjean, and Heather Stapleton, Ph.D., director of the Duke SRP Center, among others. On July 28, 2022, several committee members presented the final NASEM guidance in a public webcast.
The report “is now widely cited and used by clinicians everywhere,” Scott Masten, Ph.D., director of the Office of Portfolio Strategy in the NIEHS Division of Translational Toxicology, told Environmental Factor in 2024.
In January 2024, the CDC published PFAS Information for Clinicians, which relied on the NASEM report as a reference. The CDC guidance can be downloaded from the agency’s website, along with a fact sheet that also cites the NASEM report.
Additionally, the CDC developed a tool for estimating PFAS blood levels, intended for members of communities exposed to PFAS through their drinking water. The tool uses mathematical models based on research published in 2023 and 2022 by SRP-funded investigator Weihsueh Chiu of TAMU.
SRP Staff Expertise
NIEHS SRP staff provide subject matter expertise in discussions and decision-making about PFAS and health. In June 2024, for example, SRP health science administrator Heather Henry, Ph.D., and health specialist Brittany Trottier, Ph.D., attended the fourth National PFAS Conference, hosted by the Michigan State University (MSU) SRP Center in Ann Arbor. The conference, co-chaired by Courtney Carignan, Ph.D., of the MSU SRP Center, gathered community groups, researchers — including various SRP grant recipients — and public officials to discuss PFAS challenges and strategies to protect community health.


