By Adeline Lopez
NIEHS Superfund Research Program (SRP)-funded scientists at the previously funded University of California, Davis Center have translated basic research in insects and rodents into promising new therapies and pain treatment options for dogs, horses, and humans. This work has been spearheaded by Bruce Hammock, Ph.D., who led the center for over three decades.
The Problem
Exposure to hazardous substances in the environment can affect animal and people's health in a variety of ways, contributing to or worsening conditions such as respiratory or cardiovascular diseases, diabetes, obesity, neurological disorders, or even cancer. Understanding how these agents trigger biological responses that lead to disease is critical to designing new approaches to reduce their toxicity and improve health.
SRP Solutions
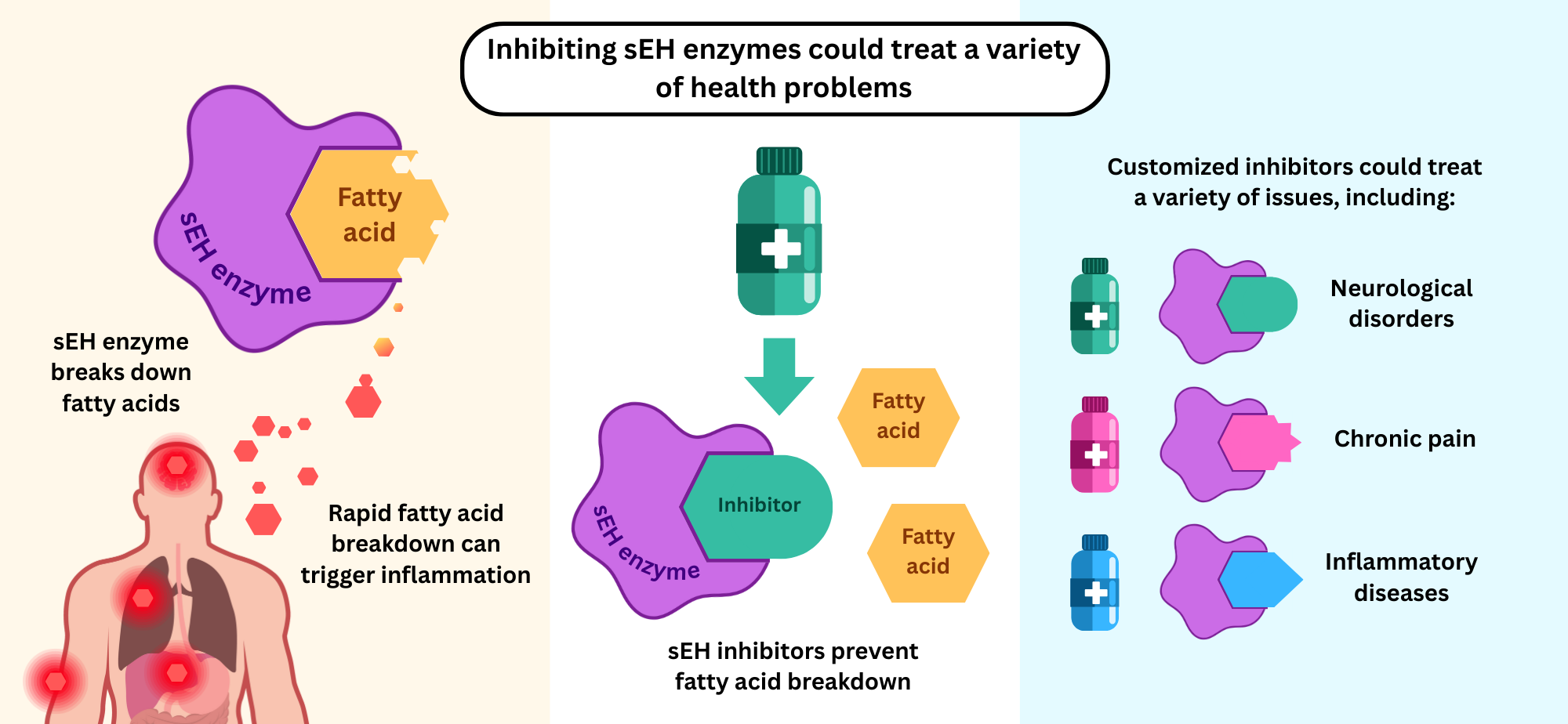
Hammock and his team are renowned for their discovery of soluble epoxide hydrolase (sEH), an enzyme in the body that breaks down fatty acids. Fatty acids are nutrients that have many important functions in the body, such as regulating biological processes or being involved in the body's inflammatory response.
Trained as an entomologist and toxicologist, Hammock's early years were spent studying how caterpillars become butterflies, a process called metamorphosis, to design greener pesticides that interfere with that process. As a graduate student funded in part by NIEHS, Hammock and fellow student Sarjeet Gill, Ph.D., discovered sEH and its important role in metamorphosis by degrading the caterpillar's juvenile hormones.
"Sarjeet and I began to wonder if the enzyme occurs in plants, other animals, or humans and what other processes it was involved with," recalled Hammock. "We had no idea where it was going to lead, but we continued to follow the science for the next several decades. It's been so rewarding to see this line of questioning start to have a real and positive impact."
Revealing the Benefits of Blocking sEH
"After we learned a bit about how the sEH enzyme works, we began to develop tools to block its function so we could learn more about what it does," Hammock shared.
To study the role of sEH to detoxify environmental chemicals, his team created potent inhibitors to investigate factors that control enzyme activity. Through these studies, they discovered it can be useful to block the function of sEH so that beneficial fatty acid epoxides, like those from omega-3 and omega-6, are not degraded.
"It turns out, sEH is involved in a very fundamental pathway called endoplasmic reticulum [ER] stress," Hammock explained. "The ER stress response, which increases or decreases inflammation and cell death depending on the situation, underlies many different diseases. We found that taking advantage of this common thread and inhibiting sEH can reduce and resolve inflammation associated with a diverse group of diseases."
Wide-Ranging Health Applications
Hammock is a Distinguished Professor with joint appointments with the UC Davis Department of Entomology and Nematology and the Comprehensive Cancer Center. Hammock joined the UC Davis faculty in 1980.
(Photo courtesy of UC Davis)
Hammock and team showed how blocking sEH can potentially treat a variety of health problems:
- Respiratory health: Reduces inflammation and airway hyperresponsiveness, decreases oxidative stress related to asthma, and protects against lung injury from air pollution exposure.
- Cardiovascular health: Prevents damage to the heart, including protecting against high blood pressure, atherosclerosis, and arrythmias.
- Kidney health: Reduces kidney damage and inflammation associated with obesity and diabetes. They also revealed potential therapeutic agents to treat kidney failure.
- Liver protection: Lessens the harmful effects of chemicals on the liver, preventing liver damage.
- Gut health: Protects against inflammatory bowel disease, obesity-related leaky gut, and gut-injury resulting from high sugar consumption.
- Cancer and chemotherapy side effects: Reduces inflammation caused by chemotherapy, preventing pancreas and liver cancer from spreading.
- Brain and neurological health: Shows promise for treating inflammation in the brain and neurological diseases and disorders, including stroke, seizures, depression, Parkinson's Disease, diabetes-related dementia, Alzheimer's Disease, and an age-related eye disorder called macular degeneration.
- Metabolic disease: Protects against inflammation and metabolic diseases, including diabetes and metabolic-related liver disease.
"I know it sounds almost like a snake oil, but it seems that controlling sEH can cure whatever ails you," Hammock joked.
One of the most promising applications to emerge for sEH therapies is related to pain. Hammock's team found that inhibiting sEH can treat chronic pain associated with human diabetic neuropathy, laminitis in horses, inflammation in rats, and osteoarthritis in dogs.
"Neuropathic pain largely is an untreatable disease, or it used to be,"said Hammock. "We saw this unmet medical need and really wanted to do something to make a difference. We've also done a lot of work with companion animals, who also experience pain, and horses with severe laminitis."
From Discovery to Drug Development
To translate these findings into treatments, Hammock and collaborators founded EicOsis LLC, a small business dedicated to developing drugs to treat pain in human and animals. Funded in part by NIEHS, EicOsis derives its name from eicosanoids - the lipid signaling molecules involved in the body's inflammatory response - and epoxide - a key chemical group targeted by sEH inhibitors.
Their sEH inhibitors are more effective at reducing inflammation and inflammatory pain compared to traditional anti-inflammatory drugs.
Their lead drug candidate, EC5026, has proven safe in clinical trials:
- 2019: Received clearance from the U.S. Food and Drug Administration for a clinical trial in healthy volunteers.
- 2020: Granted fast-track designation for treatment of neuropathic pain and successfully completed a Phase 1a clinical trial with no drug-related adverse effects.
- 2024: Completed a Phase 1b clinical trial, showing the drug works well as a once-daily oral treatment.
- The next step: EicOsis plans to initiate patient trials in people with neuropathic pain from spinal cord injuries.
According to the team, EC5026 may help treat conditions like neuropathic pain, arthritis, and neurodegenerative diseases, offering an important alternative to opioid analgesics. Beyond pain, the team is exploring other sEH-inhibiting drugs for Alzheimer’s disease, subarachnoid hemorrhage, and cardiovascular inflammation.
"Translation is critical, but it is always important to realize that the most significant translational science we do in the university is fundamental research," said Hammock. "That is the backbone of everything we do to protect and improve public health."
Long-Term Support for Innovation
NIEHS first funded Hammock’s research in 1975. For over nearly five decades, support from SRP and the NIEHS Revolutionizing Innovative, Visionary Environmental Health Research program has allowed his team to pursue new directions and move discoveries from the lab into clinical trials.
"This long-term funding from NIEHS has been instrumental in our discovery of soluble epoxide hydrolase and its role in inflammation and pain," said Hammock. "Our therapeutic targets are now advancing through clinical trials, which is a testament to how foundational science, supported consistently, can evolve into real-world health-protective treatments."


