May 09, 2022

An educational approach that blends lectures and hands-on molecular modeling can improve nurses’ understanding of the interplay between environmental health and genetics in Native American communities, according to a recent study funded by NIEHS.
The team included researchers from the Massachusetts Institute of Technology’s (MIT) Center for Environmental Health Sciences and New York University’s Langone Center for the Investigation of Environmental Hazards — both Core Centers — and the University of New Mexico’s Health Sciences Center, in collaboration with Missouri Breaks Industries Research, Inc., and nursing students and nursing professionals serving tribal nations in New Jersey and South Dakota.
Their study reflects a national effort to improve precision medicine, the practice of tailoring prevention and treatment strategies to an individual’s unique genetic makeup and exposures to environmental contaminants.
“People from different world heritages can have specific vulnerabilities to environmental exposures,” said author Kathleen Vandiver, Ph.D., director of community outreach and education for MIT’s Core Center and its Superfund Research Program Center. “Our learning framework builds awareness among nurses about how the environment can affect their patients’ health.”
An Environmental Justice Perspective on Health
Indigenous communities struggle with many chronic illnesses, such as cardiovascular diseases and several types of cancers, and endure frequent exposures to environmental contaminants. For example, an estimated 600,000 Native Americans live near more than 160,000 abandoned hard-rock mines that potentially contain contaminants harmful to health, including arsenic, cadmium, and uranium, among others.
“Nurses comprise the largest single health care professional group in the world,” Vandiver said. “They can play a pivotal role in communicating health information to communities like these in culturally appropriate languages.”
For their study, the researchers partnered with 116 nursing students and nurses in New Jersey and South Dakota who support public health programs for members of the Ramapo Lenape Tribe and the Cheyenne River Sioux Tribe, respectively.
Learning by Doing
The team’s educational approach centers on modeling kits used to build 3D representations of DNA, RNA, and proteins.
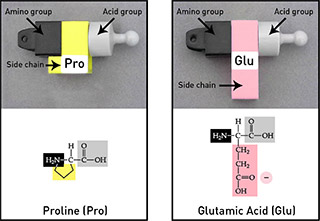
“Each plastic piece is color-coded to symbolize a molecular component,” said Vandiver, who designed the models in collaboration with MIT’s Edgerton Center. “Students can easily manipulate assembled structures to study different concepts.”
Participants first familiarized themselves with the models by completing basic lessons in molecular biology, such as how RNA is used to make proteins, and how amino acid sequence affects protein function.
Attention then turned to the critical role that genetics can play in people’s susceptibility to environmental exposures. Specifically, participants examined the role of cytochrome P450 proteins, a family of proteins found in the liver and kidneys that can break down toxic substances and drugs, but that can also convert some molecules into DNA-damaging products.
Different populations have variations in cytochrome proteins that affect their ability to bind and break down certain contaminants. To drive home that lesson, the researchers presented three hypothetical people, each with a different cytochrome variant, including one commonly found in Native American populations.

Using the models, participants investigated how each protein variant interacted with drugs or toxic substances, represented by paper shapes. For example, the nurses discovered that the variant common in Indigenous populations quickly bound and broke down nicotine, the addictive chemical in cigarettes.
“Smokers with that variant would probably experience intense cravings for nicotine, as the high is short-lived,” Vandiver explained.
Those individuals would also be more vulnerable to cancer, the participants learned. The same protein variant also binds a particular chemical found in cigarette smoke and transforms it into a cancer-causing agent.
“By going through each case study using the models, the students saw that genetic variations in cytochrome proteins can affect human behavior as well as cancer risk,” Vandiver said.
The researchers coupled the model-building exercises with three 40-minute lectures that incorporated research conducted in partnership with Indigenous community members in the U.S.
The lectures — taught by Judith Zelikoff, Ph.D., of New York University and Esther Erdei, Ph.D., of the University of New Mexico — covered introductory concepts in environmental health and toxicology; intervention strategies for marginalized communities facing environmental contamination; and the biology behind how our bodies metabolize toxic environmental substances.
“Experiencing a combination of educational methods — in this case, hands-on modeling and lectures — is a much more wholesome way of learning,” Vandiver said.
Making Strides
To test participants’ knowledge gains, Vandiver and colleagues administered pre- and post-study tests.
Results were encouraging. For example, before the lessons, only 80% of participants recognized proteins as essential parts of cells. That number jumped to 91% afterward. Similarly, post-project, nearly all participants correctly answered a question about the role of genetic heritage in a person’s susceptibility to environmental contaminants, up from 84%.
The research builds on an earlier study that Vandiver and colleagues conducted at MIT that showed similar improvement among practicing nurses.
“Together, these findings point to wide applicability of our hands-on framework, including as part of continuing education courses for nurses and other medical professionals,” Vandiver said.
Vandiver herself will soon engage in continuing education as a participant in the NIEHS-funded Environmental Health Research Institute for Nurse and Clinician Scientists, a program that equips participants with skills necessary to enhance their work in the medical field.
“The whole idea behind the program is to improve ways to teach nurses and other clinicians about environmental health,” Vandiver said. “This is exactly where I wanted to go with my work, and I’m really excited.”


