Understanding What People Think and Do About Well Water Contamination
Measuring community members’ understanding of environmental health topics and self-efficacy to act on that knowledge can help researchers and educators better tailor interventions to meet the needs of communities. A team of NIEHS-funded researchers at the University of North Carolina at Chapel Hill, the University of Kentucky, and the University of Arizona, worked with residents who were concerned about their well water quality.
They developed an environmental health literacy (EHL) assessment instrument that is unique because it measures not only environmental health knowledge, but also factors that influence health behaviors. The scale examines residents’ beliefs in their ability to put knowledge into practice, or their self-efficacy, to reduce risk of poor health outcomes from contaminated well water. A September paper describes how this team developed and used the EHL instrument.
“We wanted to develop an instrument that went beyond knowledge assessment, to incorporate factors like self-efficacy,” stated Kathleen Gray, Ph.D., lead author and director of the Community Engagement Cores of the NIEHS-funded University of North Carolina Environmental Health Sciences Core Center and Superfund Research Center. “Self-efficacy data can provide greater context for understanding how people act on information about environmental health risks. When we started the study, beliefs were not incorporated into existing EHL instruments, giving us an opportunity to add that component.”

University of North Carolina at Chapel Hill (UNC) Community Engagement Core members who lead community engagement and research translation activities. From left: Dana Haine, Andrew George, Ph.D., Kathleen Gray, Ph.D., Neasha Graves, Sarah Yelton, and Megan Lane. (Photo courtesy of Emily Williams)
Developing the Environmental Health Literacy Instrument
The researchers modeled their well water EHL instrument on a validated health literacy instrument called Newest Vital Sign. This validated instrument asks test-takers to review a nutrition label and answer a series of questions that examine how well they understand the label and nutrition concepts. Researchers similarly used a scenario-based format for the well water project, in which the scenario is a family deciding whether to use water that has arsenic in concentrations that exceed federal action levels. The EHL instrument contained four components:
- The hypothetical family scenario.
- A hypothetical report describing arsenic levels in the family home and in the neighborhood.
- A handout with information about arsenic and how it affects health.
- Questions focused on understanding of arsenic exposure and information-seeking behavior.
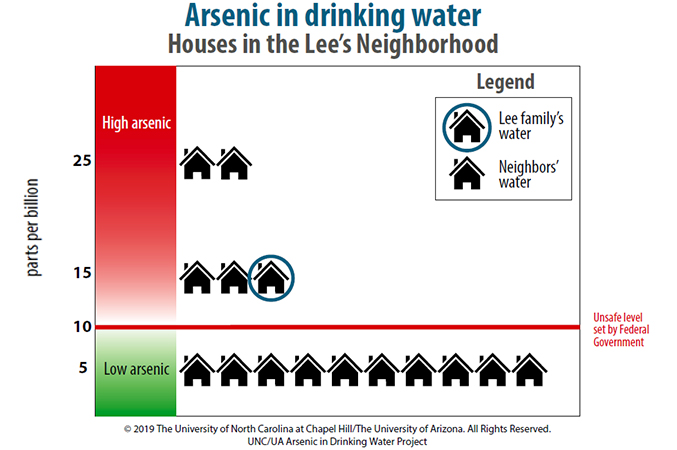
The hypothetical report of arsenic in the family home. (Photos courtesy of Emily Williams)
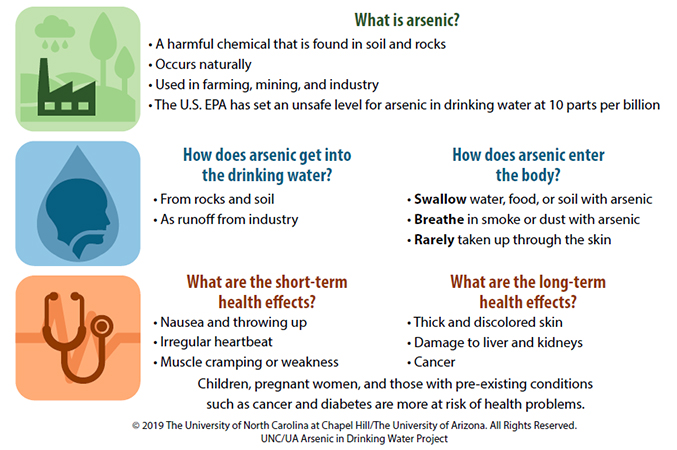
Handout with information about arsenic. (Photos courtesy of Emily Williams)
In addition to these four components, researchers also administered a self-efficacy survey which examined participants’ beliefs in their ability to test and treat well water and find environmental health information. For example, the survey asked about whether participants felt able to take the steps necessary to install a water filter in the home to remove contaminants.
“Researchers typically measure knowledge when assessing EHL, but information on other factors that influence behavior is also critical to understanding how people will respond when confronting potentially harmful environmental exposures,” added Gray. “The self-efficacy survey provided insight into participants' beliefs in their ability to act on their environmental health knowledge.”
Testing the Environmental Health Literacy Instrument
Researchers tested the EHL instrument with 23 residents of communities with toxic metals contamination in well water and 24 undergraduate students who were not majoring in scientific disciplines. Researchers gave participants the scenario and report, and then participants answered a series of questions to examine how well they understood the environmental health concepts. Participants were then given a handout which provided information on arsenic and its health effects. After reviewing the handout, participants were able to answer the questions again. Additionally, by calculating EHL scores and comparing results with health literacy scores from the validated Newest Vital Sign instrument, the researchers gained insight into how EHL and health literacy may be related.
The instrument revealed differences in environmental health knowledge and self-efficacy between the community members and students. Students had higher EHL and health literacy scores, while community members indicated greater self-efficacy to take actions such as getting water test kits or installing filtration systems. These data were further supported by focus group discussions. While students demonstrated broader knowledge of environmental health topics in discussion, residents were better able to describe what they could do to reduce their risk of adverse health outcomes.
Researchers hypothesized that the differences between the groups may be related to greater lived experience among community members for whom the issue of arsenic contamination is more pressing. Residents may also have more resources than do students to purchase tests and filters. Additionally, higher assessment scores among students may reflect their active involvement in formal education, where testing is common.
“Tailoring interventions to communities’ needs is critical,” reflected Gray. “And as we seek to measure the impact of interventions, it is important to gather robust data that reflects what we know about behavior. Importantly, by including self-efficacy in our study, we demonstrated the value of considering how people would act on knowledge and key constraints to action. For well testing, financial resources and distance to travel to get well testing materials proved to be important constraints.”
Gray noted that another benefit of this project was the opportunity to expand the field of people working on EHL by involving young researchers and students.
“Working on this project was my first experience with research from start to finish,” said Victoria Triana, currently a student at the University of North Carolina’s Gilllings School of Global Public Health. “It solidified my decision to pursue a Master of Public Health, so I could gain further skills and continue to improve the accessibility of environmental health information for community audiences.”
The researchers continue to engage with communities concerned about arsenic exposure and seek to better understand how knowledge and beliefs interact to influence outcomes. For example, in a February 2022 paper, Gray and colleagues describe how residents implemented well water filtration and residents’ perceived barriers to doing so. The team hopes their work on EHL will lead to more effective educational interventions that ultimately reduce harmful environmental exposures among people who use well water.
Educational Framework Increases Environmental Health Literacy Among Nurses
An NIEHS-funded team, working with Tribal partners, published a paper in January about an innovative educational framework for building environmental health literacy among health care providers who serve vulnerable communities. The pilot project was driven by the team’s belief that the education of health professionals is essential in improving community health. It combined hands-on modeling exercises with case-based lessons and lectures on toxicology that focused on community-based environmental health research. Participants, who were nurses and nursing students serving Native Americans in both rural and urban areas, had substantial knowledge gains and a greater understanding of genetic susceptibility to environmental health risks after the program. The framework can be used in many settings, including health care organizations that work with populations exposed to long-term hazardous environmental risks, according to the authors.
New Public Information Series Provides Actionable Information on Climate-related Health Risks
The U.S. Office of Climate Change and Health Equity launched a new public information series, the Climate and Health Outlook, in May. Each installment in the series connects weather and climate forecasts from the National Oceanic and Atmospheric Administration to actionable information so that individuals, health care professionals, and public health officials can take action to reduce health risks associated with climate-related hazards such as wildfires, hurricanes, and droughts.
May’s inaugural edition focused on extreme heat. It presents estimates of which U.S. counties are expected to experience extremely hot days this summer and identifies vulnerable populations that are at high risk from extreme heat. It also describes how heat affects health and provides practical resources for people at high risk of heat-related health problems. These resources include information on how to prevent heat illness at work, a listing of federal programs that assist families with improving indoor temperatures, best practices for emergency managers, and clinical best practices. The second edition, which was an update to the first, was released in June and focuses on temperature predictions from June through August 2022.
NIEHS-funded Researchers Focus on Solutions-oriented Risk Communication
A team of NIEHS-funded researchers at the University of Arizona and a public water department developed a communication model that improves risk communication. The researchers used concepts from environmental health literacy, such as understanding the literacy levels of target audiences and how to address misperceptions by using plain language, to inform the creation of the model for developing risk communication messages and materials. To build the model, they also gathered data from focus groups to determine how people perceive risk, their communication preferences, and how they respond to materials developed using the model. Part of the work also focused on training communicators to create information that better helps the public protect themselves and their families. Overall, the article proposes new best practices for engaging with audiences about environmental health risks, including developing a profile of the community in advance of an emergency so that new, effective communication can be developed and deployed quickly when needs arise.
Public Health Tools for Communicating Through the Pandemic and Beyond
The Public Health Communications Collaborative put out a new resource, Communicating Through COVID-19 and Beyond, based on a survey that collected information from public health workers about communication through the pandemic. More than 600 respondents, including commissioners, public information officers, community health workers, contact tracers, educators, program directors, and nurses, answered the survey. The resource includes survey results, tips for public health communication, and short spotlight articles from public health professionals on their professional experiences during the pandemic. Topics include health literacy, community outreach, and health equity. Three of the spotlight communicators also gave a webinar in April that went into more detail about the learnings from their departments’ COVID-19 communications strategies.
U.S. Commits to Initiative on Climate-resilient and Low Carbon, Sustainable Health Systems
U.S. Commits to Initiative on Climate-Resilient and Low Carbon, Sustainable Health Systems The World Health Organization’s COP26 Health Programme aims to protect the health of people and the planet by supporting initiatives such as building climate-resilient health systems and developing low carbon sustainable health systems, among others. The U.S. Department of Health and Human Services (HHS) announced its commitment to the program last year, indicating that it will conduct climate change and health vulnerability and adaptation assessments, develop a health National Adaptation Plan, deliver a baseline assessment of the health system’s greenhouse gas emissions, and develop an action plan to develop a sustainable low carbon health system. In an April 2022 perspective published in the New England Journal of Medicine, John Balbus, M.D., M.P.H., interim director of the Office of Climate Change and Health Equity, and others outlined broad policy areas on which HHS will work to meet its commitment to address the health threats associated with climate change equitably and inclusively.

PEPH Grantee Highlight
Karletta Chief, Ph.D.
Growing up within the Navajo nation and being affected by coal mining pollution led Karletta Chief, Ph.D., to her interest in studying water. As a hydrologist at the University of Arizona, she now helps improve environmental health by facilitating collaborations between Indigenous communities and researchers. Chief is the Community Engagement Core lead for the NIEHS-funded Superfund Research Center and the director of the Indigenous Resilience Center, both at the University of Arizona. Her work focuses on addressing the impacts of environmental contamination and climate change on tribal water sources. Read more about Chief’s work in the January 2022 PEPH newsletter.
Funding Opportunities
SBIR E-Learning for HAZMAT and Emergency Response (R43/R44 Clinical Trial Not Allowed)
Encourages Small Business Innovation Research (SBIR) grant applications from small business concerns that propose to further the development of Advanced Technology Training (ATT) products for the health and safety training of hazardous materials (HAZMAT) workers; waste treatment personnel; skilled support personnel associated with an emergency/disaster; emergency responders in biosafety response, infectious disease training and cleanup; emergency responders in disasters and resiliency training; and for ATT tools to assist in responding to environmental disasters. The major objective of the NIEHS Worker Training Program (WTP) is to prevent work related harm by assisting in the training of workers in how best to protect themselves and their communities from exposure to hazardous materials. NIEHS encourages applicants to review the SBIR E-Learning for HAZMAT Program, to pursue partnerships and collaboration with awardees of the WTP program, and to design new technology-enhanced training methods or e-Learning products that can enhance the existing NIEHS supported curricula and training programs while adhering to the Minimum Health and Safety Training Criteria: Guidance for Hazardous Waste Operations and Emergency Response (HAZWOPER) and HAZWOPER-Supporting Training.
Deadline: July 30, 2021
Letter of Intent: June 30, 2021
Implementation Research to Reduce Noncommunicable Disease Burden in Low- and Middle-income Countries and Tribal Nations During Critical Life Stages and Key Transition Periods (R01 Clinical Trial Optional)
Supports innovative approaches to identifying, understanding, developing, and implementing strategies for overcoming barriers to the adoption, adaptation, integration, scale-up, and sustainability of evidence-based interventions, tools, policies, and guidelines. In addition, studies to advance dissemination and implementation research methods and measures into application are encouraged. Specifically, this FOA invites applications that propose interventions targeting critical life stages (e.g., infancy, childhood, adolescence, pregnancy, older adults) and key transitions between life stages to reduce health risk and/or enhance positive health and lifestyle behaviors. NIEHS is interested in applications that focus on the implementation of interventions that address environmental noncommunicable disease risk factors (e.g., air pollution, disaster risks attributed to climate change, etc.) in one or more critical life stages.
Deadline: July 27, 2022
Notice of Special Interest (NOSI): Climate Change and Health
Encourages applications that address the impact of climate change on health and well-being over the life course, including the health implications of climate change in the United States and globally. NIEHS is leading the NIH-wide Climate Change and Health Initiative, of which this NOSI is a part. NIEHS is interested in research that addresses the impact of climate change on environmental health and innovative approaches to the development of prevention and intervention strategies to reduce the impacts of climate change on environmental health, particularly in communities most susceptible to these impacts. Researchers who wish to submit applications regarding this NOSI must select from a list of funding opportunity announcements sponsored by various NIH institutes and centers. Researchers interested in applying for climate change-related Small Business Innovation Research funding can see Notice of Special Interest (NOSI): Innovative Technologies for Research on Climate Change and Human Health (R43/R44 Small Business Innovation Research (R43/R44 Clinical Trial Optional). Researchers interested in applying for climate change-related Small Business Technology Transfer funding can see Notice of Special Interest (NOSI): Innovative Technologies for Research on Climate Change and Human Health Small Business Technology Transfer (R41/R42 Clinical Trial Optional).
Deadlines: August 8, 2022; October 5, 2022; November 3, 2022
Research Coordinating Center to Support Climate Change and Health Community of Practice (U24 Clinical Trial Not Allowed)
Solicits applications from eligible institutions to develop a Research Coordinating Center (RCC) to support the development of an NIH climate change and health (CCH) community of practice by managing and supporting current and future climate change and health research and capacity building efforts. The RCC will create a robust, inclusive CCH community of practice that fosters collaboration, capacity building, innovation and research that aligns with the NIH CCH initiative. The RCC will offer opportunities for collaboration between multiple disciplines required to conduct solutions-driven research on the health impacts of climate change. Additionally, the RCC seeks to promote inclusion of scientists from diverse backgrounds, including scientists from nationally underrepresented groups (see, Notice of NIH's Interest in Diversity, NOT-OD-20-031), and Historically Black Colleges and Universities, Tribal Colleges and other Minority Serving Institutions in the community of practice. Comprehensive initiative coordination, including supporting services such as data and project management, will be part of the RCC efforts.
Deadline: August 25, 2022
Letter of Intent: July 25, 2022
PHS 2022-2 Omnibus Solicitation of the NIH, CDC and FDA for Small Business Innovation Research Grant Applications (Parent SBIR [R43/R44] Clinical Trial Not Allowed)
Enables U.S.-owned and operated small businesses to conduct research and development that has a strong potential for commercialization. This award and the associated PHS 2022-2 Omnibus Solicitation of the NIH and CDC for Small Business Innovation Research Grant Applications (Parent SBIR [R43/R44] Clinical Trial Required) provide funds for small businesses to stimulate technological innovation in the private sector and strengthen the role of small business in meeting federal research and development needs. The related Small Business Technology Transfer announcements (PHS 2022-2 Omnibus Solicitation of the NIH for Small Business Technology Transfer Grant Applications (Parent STTR [R41/R42] Clinical Trial Not Allowed) and PHS 2022-2 Omnibus Solicitation of the NIH for Small Business Technology Transfer Grant Applications (Parent STTR [R41/R42 Clinical Trial Required)) aim to foster technology transfer through cooperative research and development between small businesses and research institutions.
Deadlines: September 5, 2022; January 5, 2023; April 5, 2023
Accelerating the Pace of Child Health Research Using Existing Data From the Adolescent Brain Cognitive Development (ABCD) Study (R01-clinical Trial Not Allowed)
Supports activities proposing to conduct analyses of existing ABCD Study data to accelerate the pace of research on child health and development, including: cross-sectional and/or longitudinal analyses; development of new or advanced statistical methods; and/or integration of ABCD data with other existing datasets that share common data elements. NIEHS is interested in applications that will use ABCD data resources to examine the contribution of environmental exposures on brain and development and to identify sensitive time windows of development that may confer individual susceptibility and also to identify protective factors that may mitigate environmental-induced changes. An R21 funding opportunity is also open.
Deadlines: June 5, 2022; October 5, 2022; February 5, 2023
Research Enhancement Award Program (REAP) for Health Professional Schools and Graduate Schools (R15 Clinical Trial Not Allowed)
The REAP program will enable qualified scientists to receive support for small-scale research projects. It is anticipated that investigators supported under the REAP program will benefit from the opportunity to conduct independent research; that the grantee institution will benefit from a research environment strengthened through REAP grants; and that students at recipient institutions will benefit from exposure to and participation in scientific research in the biomedical sciences so that they consider careers in biomedical research. The REAP funding opportunity emphasizes the engagement and inclusion of health professional, undergraduates, and/or graduate students in research. Since diversity strengthens the research environment, REAP grantees are encouraged to recruit and include students from diverse backgrounds, including those from groups underrepresented in the biomedical research workforce. NIEHS will accept applications describing research projects that will have a defined impact on the environmental health sciences and must have a research focus on exposure-health related responses from environmental agents within the mission interest of the NIEHS.
Deadlines: June 25, 2022; October 25, 2022









