Climate Change and Human Health

The impacts of climate change affect everyone and can strain many aspects of our lives, including our health. However, the extent to which individuals, societies, and nations experience the adverse health impacts of climate change will vary depending on their ability to adapt to the stressors imposed by climate change. Certain populations will bear a disproportionate burden of the adverse health outcomes as a result of climate change. An understanding of these populations of concern and what underpins their vulnerability can help to inform the appropriate societal and global responses needed to curb adverse health outcomes.
Populations of Concern
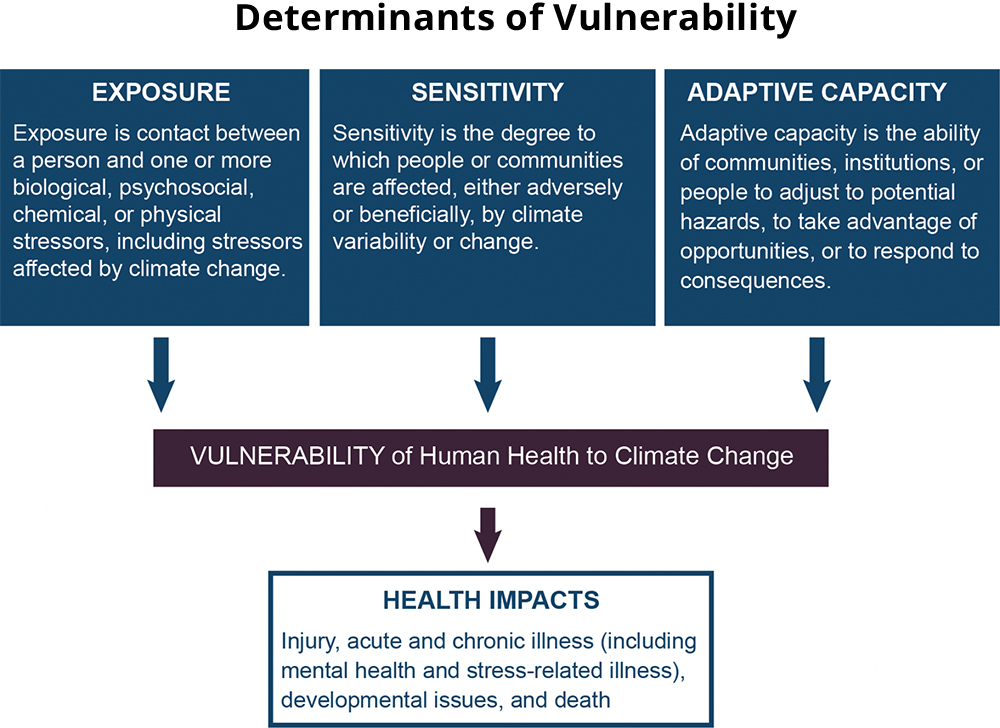
The extent of impact on a group of people can be determined by exposure, sensitivity, and adaptive capacity. Exposure refers to the contact between an individual and a climate-related hazard such as high temperatures or air pollution. Sensitivity refers to the degree to which the individual is affected by a climate change exposure and may vary depending on the individual’s life stage, existing medical problems, nutrition, and other factors. Adaptive capacity refers to an individual’s or community’s ability to evade or cope with exposure to a climate hazard.
In general, children and pregnant women, older adults, certain occupational groups, persons with disabilities, and persons with chronic medical conditions are more vulnerable to health stressors, such as extreme heat, floods, poor air quality, and other climate-related events1 , 2 , 3 . For example, children with underdeveloped immune systems may have increased sensitivity to airborne allergens. Individuals with outdoor occupations may be at greater risk of negative health consequences of extreme heat. Persons with asthma or chronic obstructive pulmonary disease may be more sensitive to air pollution. Older adults with limited mobility are less likely to adapt or physically respond to an extreme weather event.
Social, environmental, political, and economic factors can contribute to health disparities that may have greater impacts on people who are vulnerable to the impacts of climate change4 , 5 . These factors include poverty, racial discrimination, a lack of access to healthcare, inadequate education, and an unhealthy or unsafe built environment. Collectively, these factors are referred to as social determinants of health. Social determinants of health can occur simultaneously with the effects of climate change, like increased temperatures, precipitation changes, and extreme weather events, and the environmental stressors they produce, like disruptions to land-use, ecosystems, or agricultural production.
Opportunities for Public Health Improvement
A holistic approach to address the effects of climate change on human health starts with an understanding of people who are at increased risk. Vulnerability assessments that examine the intersection of environmental and social impacts can be used to improve a community’s adaptation and resilience and reduce the health impacts from climate change. Engaging communities in assessing or planning interventions that target their specific needs may also support community resilience.
Research Needs
Future vulnerability assessments can benefit from a better understanding and measurement of key population characteristics to help map vulnerability to the health impacts of climate change. Engaging with communities will ensure continued effort toward appropriate goals for each community.
Research will also be important to evaluate the efficacy of public health interventions designed to reduce the climate change-related health impacts for communities and individuals and improve resilience. Implementation science can improve strategies for promoting uptake of policies and interventions within certain population contexts.
-
Balbus JM, Malina C. Identifying vulnerable subpopulations for climate change health effects in the United States. J Occup Environ Med. 2009 Jan;51(1):33-7. doi: 10.1097/JOM.0b013e318193e12e. [Abstract Balbus JM, Malina C. Identifying vulnerable subpopulations for climate change health effects in the United States. J Occup Environ Med. 2009 Jan;51(1):33-7. doi: 10.1097/JOM.0b013e318193e12e.]
-
Luber, G., and M. McGeehin, 2008: Climate change and extreme heat events. American Journal of Preventive Medicine, 35, 429-435. [Abstract Luber, G., and M. McGeehin, 2008: Climate change and extreme heat events. American Journal of Preventive Medicine, 35, 429-435.] [Full Text Luber, G., and M. McGeehin, 2008: Climate change and extreme heat events. American Journal of Preventive Medicine, 35, 429-435.]
-
Sheffield, P. E., and P. J. Landrigan, 2011: Global climate change and children’s health: Threats and strategies for prevention. Environmental Health Perspectives, 119, 291-298. [Abstract Sheffield, P. E., and P. J. Landrigan, 2011: Global climate change and children’s health: Threats and strategies for prevention. Environmental Health Perspectives, 119, 291-298.] [Full Text Sheffield, P. E., and P. J. Landrigan, 2011: Global climate change and children’s health: Threats and strategies for prevention. Environmental Health Perspectives, 119, 291-298.]
-
Ebi, Kristie L., and Jeremy J. Hess. Health Risks Due To Climate Change: Inequity In Causes And Consequences: Study examines health risks due to climate change. Health Affairs 39.12 (2020): 2056-2062. [Abstract Ebi, Kristie L., and Jeremy J. Hess. Health Risks Due To Climate Change: Inequity In Causes And Consequences: Study examines health risks due to climate change. Health Affairs 39.12 (2020): 2056-2062.]
-
Thomas, Kimberley et al. Explaining differential vulnerability to climate change: A social science review. Wiley interdisciplinary reviews. Climate change vol. 10,2 (2019): e565. doi:10.1002/wcc.565. [Abstract Thomas, Kimberley et al. Explaining differential vulnerability to climate change: A social science review. Wiley interdisciplinary reviews. Climate change vol. 10,2 (2019): e565. doi:10.1002/wcc.565.]
-
Balbus JM, Malina C. Identifying vulnerable subpopulations for climate change health effects in the United States. J Occup Environ Med. 2009 Jan;51(1):33-7. doi: 10.1097/JOM.0b013e318193e12e. [Abstract Balbus JM, Malina C. Identifying vulnerable subpopulations for climate change health effects in the United States. J Occup Environ Med. 2009 Jan;51(1):33-7. doi: 10.1097/JOM.0b013e318193e12e.]
-
Luber, G., and M. McGeehin, 2008: Climate change and extreme heat events. American Journal of Preventive Medicine, 35, 429-435. [Abstract Luber, G., and M. McGeehin, 2008: Climate change and extreme heat events. American Journal of Preventive Medicine, 35, 429-435.] [Full Text Luber, G., and M. McGeehin, 2008: Climate change and extreme heat events. American Journal of Preventive Medicine, 35, 429-435.]
-
Sheffield, P. E., and P. J. Landrigan, 2011: Global climate change and childrenâs health: Threats and strategies for prevention. Environmental Health Perspectives, 119, 291-298. [Abstract Sheffield, P. E., and P. J. Landrigan, 2011: Global climate change and childrenâs health: Threats and strategies for prevention. Environmental Health Perspectives, 119, 291-298.] [Full Text Sheffield, P. E., and P. J. Landrigan, 2011: Global climate change and childrenâs health: Threats and strategies for prevention. Environmental Health Perspectives, 119, 291-298.]
-
Ebi, Kristie L., and Jeremy J. Hess. Health Risks Due To Climate Change: Inequity In Causes And Consequences: Study examines health risks due to climate change. Health Affairs 39.12 (2020): 2056-2062. [Abstract Ebi, Kristie L., and Jeremy J. Hess. Health Risks Due To Climate Change: Inequity In Causes And Consequences: Study examines health risks due to climate change. Health Affairs 39.12 (2020): 2056-2062.]
-
Thomas, Kimberley et al. Explaining differential vulnerability to climate change: A social science review. Wiley interdisciplinary reviews. Climate change vol. 10,2 (2019): e565. doi:10.1002/wcc.565. [Abstract Thomas, Kimberley et al. Explaining differential vulnerability to climate change: A social science review. Wiley interdisciplinary reviews. Climate change vol. 10,2 (2019): e565. doi:10.1002/wcc.565.]


