Quality Green Space Reduces Distress After Hurricanes

Spending time in green space perceived as high quality, like the natural environment or parks, can lower post-hurricane distress, according to a recent study that focused on Houston residents’ distress after Hurricane Harvey. The study results support paying more attention to neighborhoods’ green infrastructure in disaster recovery and city resilience planning.
“Exposure to a severe natural disaster is associated with increases in stress, anxiety, depression, and posttraumatic stress disorder. Access to green space can provide mental health benefits, such as decreases in stress and anxiety, and can improve physical health,” said Jennifer Horney, Ph.D., an NIEHS-funded epidemiologist and disaster researcher at the University of Delaware who collaborated on the study, which was funded through Texas A&M University’s Superfund Research Center. “But there was little research on access to greenness in the context of recovery from natural disasters, and we thought we could fill that gap.”
Hurricane Harvey, which hit the U.S. in August 2017, affected 12 million Gulf Coast residents with catastrophic flooding, displacement, and structural damage. Even a year after the hurricane, residents had mental health issues at higher levels than the U.S. average, according to a recent study.
Determining effective, wide-reaching post-disaster mitigation strategies is important for resilient city planning and equitable public health.
Surveying Houston Residents About Stress and Hurricane Exposure
Horney’s team surveyed Houston residents between August and December 2019, about two years after the hurricane. They focused on neighborhoods in which residents were heavily impacted by the hurricane and ensured their sampling was representative of socio-demographic conditions.
The team mailed survey packets and reminder postcards, and they later visited households in neighborhoods that had lower-than-average response rates. Altogether, they collected 272 valid responses, which equates to a response rate of 7.3%.
“Although the overall response rate was low, targeting neighborhoods that may have been less likely to respond was important,” reflected Horney. “These areas may also have residents who are less likely to be aware of programs that could provide support, financial or otherwise, to those impacted by Hurricane Harvey’s flooding.”
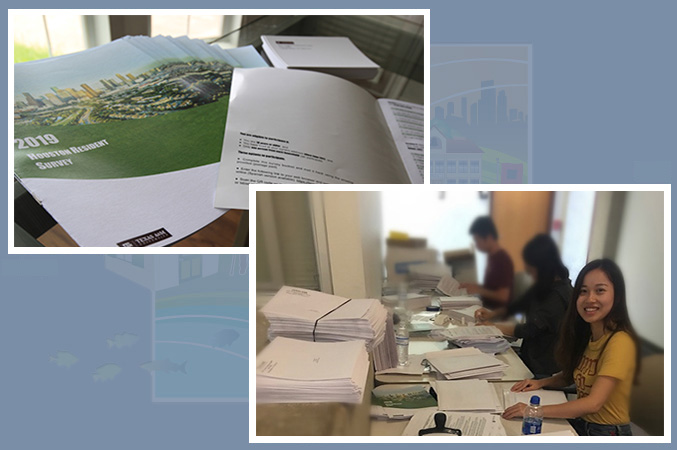
The Houston Resident Survey (top, left) and a team member working on preparing survey packets to mail to Houston residents (bottom, right). (Photo courtesy of Jennifer Horney)
The survey questionnaire asked residents to report on their experiences with the following:
- Probable post-traumatic stress disorder (PTSD)
- Hurricane-related distress
- Hurricane exposure
- Perceived quality of green space
- Emotional resilience, which is the ability of someone to adjust and recover from stress and restore well-being and positive emotions
- Neighborhood social cohesion based on inter-personal relationships
- Covariates, such as education levels, employment status, and income
Hurricane-related distress was measured by self-reported symptoms such as difficulty sleeping or concentrating. Questions related to hurricane exposure asked about stressors an individual experienced during the hurricane, such as walking through floodwaters, having severe home damage, or seeing someone die. Questions related to the perceived quality of green space touched on various aspects, such as attractiveness, accessibility, and safety, and its potential for relaxation and neighborly activities. Overall, the perceived quality of green space measurement captured the quality of the environment most relevant to participants.
The researchers also measured the concentration of neighborhood green space using aerial images from the U.S. Department of Agriculture. The concentration metric provided an objective measure of how much green space residents are exposed to, ranging from none for areas that are completely barren of vegetation to very dense green space.
“We know that many factors contribute to how well an individual recovers from a hurricane, and that they’re complex,” said Horney. “So, we wanted to control for major variables – like socioeconomic status and how severe an individual’s exposure was to the hurricane. That would let us see more clearly the potential relationships between recovery and access to quality neighborhood green space.”
The Link Between Neighborhood Green Space and Recovery
Unsurprisingly, Horney’s team found that people who reported greater exposure to hurricane stressors had higher levels of hurricane-related distress and probable PTSD. They also found that emotional resilience, perceived quality of neighborhood green space, and social cohesion were each related to lower levels of distress. Residents’ perceived quality of green space was also linked to lower levels of probable PTSD, but concentration of green space was not.
“Our findings show that the restorative benefits of nature may depend on people’s actual access to and use of the space, not just the existence of green space, which is sometimes used post-disaster for debris storage or for staging of temporary housing,” said Horney. “But outside the context of natural disasters, there’s an environmental health disparity around access to green space. Ensuring all populations have access to high-quality green space is important so everyone can benefit.”
Horney’s team hypothesized that the beneficial effect of green space on lowering probable PTSD and levels of individual distress was related either to emotional resilience or social cohesion. To figure out which, they tested different statistical models based on the survey data. They found that emotional resilience, but not social cohesion, was the link between perceived quality of green space and distress symptoms.
The study’s findings have implications for public health, disaster recovery, and planning policies and point to positive environmental exposures as aiding recovery. Promoting positive environmental exposure is important, especially since a lot of post-disaster research has focused on green space contamination by floodwater and residents’ perception of the safety of using affected green space after flooding has receded.
“Access to restorative environments such as high-quality green space should be a part of the health disparities discussions after disasters,” said Horney. “Our findings raise the possibility that community green space as a low-cost public amenity can be used to reduce inequalities and promote mental well-being and preparedness for at-risk populations.”
NIEHS Portal Empowers Human Health Research in Response to Disasters and Public Health Emergencies
The NIEHS Disaster Research Response (DR2) Program curates the DR2 Resources Portal, a repository of publicly available data collection tools and resources related to human health research in response to disasters and public health emergencies. The portal includes resources such as research protocols, survey instruments, consent forms, guidance manuals, and data dictionaries. The database can be searched through basic or advanced keyword searches, or you can browse specific collections such as disasters and reproductive health, measuring social support and resiliency, understanding impacts of hurricanes on communities, and COVID-19-related resources. You can also suggest a resource for inclusion in the portal through the resource submission form. Detailed information about how to use the portal is available in the DR2 Portal Criteria Guidance.
NIEHS Worker Training Program Resources on Disaster Preparedness and Response
The NIEHS Worker Training Program has training tools and other resources about disaster preparedness and response. Materials cover disasters such as earthquakes, hurricanes and floods, infectious diseases, oil spills, wildfires, and responder and community resilience. For example, the responder and community resilience materials were designed to educate and empower people impacted by disasters to recognize signs and symptoms of disaster work-related stress, get support through an employer or community resources, and build resilience by understanding stress reduction and coping strategies. The material, which was developed with support from the Substance Abuse and Mental Health Services Administration, is aimed at disaster workers, supervisors, and care providers.
Another section of the Worker Training Program’s material focuses on wildfire response operations. It includes tools that can be incorporated into awareness-level training for wildfire responders to protect themselves during disaster response. Additional resources include guidance on how employers can adhere to California’s worker protection from wildfire smoke safety regulation, and a fact sheet on ways wildfire responders can protect themselves during wildfire cleanups.
Preparing Institutional Review Boards to Evaluate Disaster Research Protocols
A new NIEHS-led review, Institutional Review Board Preparedness for Disaster Research: A Practical Approach, describes approaches for institutional review boards (IRBs) to evaluate disaster-related research protocols. To aid in the review of disaster research, the authors developed a Disaster Research Critical IRB Review Factors Model, which accounts for key differences between routine public health or clinical research and disaster research. The model portrays five factors specifically relevant to the review of disaster research, such as time point in the disaster management cycle and return of research results to participants and the affected community. One review factor, the status of potential research participants, is multifaceted and includes considerations such as a disaster-specific consent process and participant health and stability.
Strengthening the ethical considerations of disaster research is important. Government agencies are increasingly interested in disaster research to better respond and build resiliency. Consequently, IRBs are seeing more research protocols aimed at assessing health risks, exposures, and outcomes from disaster survivors. However, few IRBs have experience reviewing disaster research protocols, and there is a lack of guidance for IRBs regarding disaster research protocols. Moreover, people and communities affected by a disaster have unique challenges that necessitate careful consideration of how to involve them in research. The five-factor model provides a framework that emphasizes contextual factors to strengthen ethical research practices around disaster research.
New Fact Sheets About Climate, Health, and Emergency Preparedness
The National Environmental Health Association recently published seven fact sheets that cover topics related to emergency preparedness and climate change, such as air quality, drought, extreme heat, extreme storms, floods, and wildfires. The documents’ information and resources cover health effects of climate change, recommendations for reducing adverse outcomes, the role of environmental health workers in mitigating impacts of environmental health emergencies, and the importance of climate justice and health equity. For example, the air quality fact sheet has a fast facts section, a description of how poor air quality harms health, a description of the role of the environmental health workforce in preventing and reducing public health risks of air quality, and recommendations geared to environmental health professionals. The fact sheets are part of the National Environmental Health Association’s larger Climate Change collection, which also has an online community, a video about addressing the impacts of climate change, reports from an annual survey on climate change, and other resources.
NIH Requests Public Comments on Gaps in Women’s Health Research
NIH is inviting comments from the extramural scientific community, professional societies, and the general public about gaps in women’s health research and pitfalls in clinical practices. NIH asks that comments focus specifically on specific areas: increasing maternal morbidity and mortality rates, increasing rates of chronic debilitating conditions in women, and the stagnant cervical cancer survival rates. NIH is also asking for real-life testimonial experiences related to the three public health areas listed above. Comments will inform the direction and scope of the Advancing NIH Research on the Health of Women Conference, which will be held in October 2021 and will involve members of NIH and the U.S. Congress. Participants will discuss the current state of NIH-supported women’s health research, research gaps, and research opportunities. Comments are due September 15, 2021.
New Chronic Stress and Environmental Contamination Training Module
The Agency for Toxic Substances and Disease Registry (ATDSR) has launched a new Chronic Stress and Environmental Contamination Training. The self-guided online training is intended for public health professionals working with communities affected by environmental contamination, such as perfluoroalkyl and polyfluoroalkyl substances in drinking water. It covers the biology of psychological stress, reasons why environmental contamination can be a source of chronic stress, the role of community resilience, and ways to tailor public health activities to support community psychosocial health.
The training complements ATSDR’s Community Stress Resource Center, which is part of their work to better understand and develop resources to address the psychological and social impacts associated with living in a community affected by long-term environmental contamination. Please direct questions to [email protected].
NIH Seeks Input on Climate Change and Health
The NIH Climate Change and Human Health Working Group invites feedback on approaches NIH can take to enhance research on the health implications of climate change. Comments are invited from researchers, community advocates, clinicians, and policy makers. NIH is seeking information related to research gaps and priorities in six areas such as scientific infrastructure to address human health and climate change, research and community partnerships to address environmental injustice and foster resilience, and translation and dissemination of research findings and health protective strategies. Responses on related topics that are not listed are also encouraged. The deadline has been extended to September 17, 2021.

PEPH Environmental Health Chat Podcast Series
Wildfire Smoke and Children’s Health
PEPH Environmental Health Chat Podcast Series
Wildfire Smoke and Children’s Health

PEPH Grantee Highlight
Elaine Symanski, Ph.D.
Elaine Symanski, Ph.D., knows that it’s critical to meaningfully involve communities to promote social and environmental justice. As the director of the NIEHS-funded Maternal and Infant Environmental Health Riskscape Research Center; and deputy director of the NIEHS-funded Gulf Coast Center for Precision Environmental Health, she ensures her environmental health research is culturally relevant by getting community buy-in for potential solutions. In doing so, she hopes to address a lack of trust among residents, researchers, government officials, and industry stakeholders, a common barrier to addressing health concerns. For example, the Metal Air Pollution Partnership Solutions project, which was featured in the June 2020 PEPH newsletter, brought community members and metal recyclers to the table to work together. The group ultimately developed a public health action plan that led to industry partners reducing emissions from their metal recycling facilities. Symanski also works on community-engaged maternal health research. After conducting conversations with the community, her team is developing a forum for mothers to talk to researchers about their experiences and concerns around childbirth.
Funding Opportunites
Support for Research Excellence – First Independent Research Award (R16 Clinical Trial Not Allowed)
The purpose of the Support for Research Excellence – First Independent Research (SuRE-First) awards is to support research grants for faculty investigators who have not had prior independent external research grants. A SuRE-First applicant must identify a scientist based in the U.S. with expertise and an extramural funding record in the proposed field of research to serve as a mentor. SuRE-First-supported projects must have student participation in the execution, analysis, and reporting of the research. Awards are open to institutions that receive no more than $6 million per year from NIH Research Project Grants and additionally enroll at least 25% of undergraduate students supported by Pell grants, or are an accredited medical/health professional school with a historical mission statement that explicitly states that it was founded to educate students from nationally underrepresented backgrounds.
Deadlines: September 28, 2021; September 28, 2022; September 28, 2023
Addressing Health Disparities Among Immigrant Populations Through Effective Interventions (R01 Clinical Trial Optional)
Supports research to design and implement effective interventions to enhance health advantages and reduce the health disparities among U.S. immigrant populations, particularly migrant workers, recent and first-generation immigrants. This announcement calls for multidisciplinary/multilevel research focusing on the design and implementation of effective interventions that will address immigrant-specific factors to reduce health disparities. A framework to demonstrate the multidomain, multilevel factors that may influence health disparities is available here. A life-course perspective is encouraged with interventions focusing attention on transition points across the lifespan and associated risk and protective factors for immigrant populations. Projects should involve collaborations among relevant stakeholders in U.S. immigrant population groups, such as researchers, community organizations, healthcare providers, public health organizations, consumer advocacy groups, and faith-based organizations. Projects must focus on immigrants from one or more NIH-designated populations that experience health disparities in the U.S., which include racial and ethnic minorities (Blacks or African Americans, Hispanics/Latinos, Asian Americans, and Pacific Islanders).
Deadlines: February 5, 2021; June 5, 2021; October 5, 2021
Addressing the Etiology of Health Disparities and Health Advantages Among Immigrant Populations (R01 Clinical Trial Not Allowed)
Supports innovative research to understand factors uniquely associated with the immigration experience that contribute to health disparities or health advantages among U.S. immigrant populations, particularly migrant workers, recent and first-generation immigrants. This announcement calls for multidisciplinary research to address the specific underlying causes and mechanisms of health disparities and health advantages. A framework to demonstrate the multidomain, multilevel factors that may influence health disparities is available here. Projects should involve collaborations among relevant stakeholders in U.S. immigrant population groups, such as researchers, community leaders and organizations, public health organizations, consumer advocacy groups, faith-based organizations, and healthcare providers. Projects must focus on immigrants from one or more NIH-designated populations that experience health disparities in the U.S., which include racial and ethnic minorities (Blacks or African Americans, Hispanics/Latinos, Asian Americans, and Pacific Islanders).
Deadlines: February 5, 2021; June 5, 2021; October 5, 2021
Dissemination and Implementation Research in Health (R01 Clinical Trial Optional)
Supports innovative approaches to identifying, understanding, and developing strategies for overcoming barriers to the adoption, adaptation, integration, scale-up and sustainability of evidence-based interventions, tools, policies, and guidelines. Additionally, there is a benefit in understanding circumstances that create a need to stop or reduce (“de-implement”) the use of interventions that are ineffective, unproven, low-value, or harmful. This FOA invites research grant applications that will identify, develop, test, evaluate, and/or refine strategies to disseminate and implement evidence-based practices (e.g. behavioral interventions; prevention, early detection, diagnostic, treatment and disease management interventions; quality improvement programs) into public health, clinical practice, and community (e.g., workplace, school, place of worship) settings. Studies to advance dissemination and implementation research methods and measures are also encouraged.
Deadlines: February 5, 2021; June 5, 2021; October 5, 2021
Letter of Intent: Due 30 days prior to the application due date
Pediatric Immune System – Ontogeny and Development (INTEND) (R01 Clinical Trial Not Allowed)
Supports research which correlates immune system in general and development patterns in particular, between two or more age groups - neonates, infants, and children and adolescents to understand the evolution or immune ontogeny in human immune system development focusing on either or both, innate and adaptive immune systems with additional focus on internal factors like the microbiome and/or external factors like the environment.
Deadlines: October 5, 2021; February 5, 2022
The Role of Work in Health Disparities in the U.S. (R01 Clinical Trials Optional)
Supports innovative population-based research that can contribute to identifying and characterizing pathways and mechanisms through which work or occupation influences health outcomes and health status among populations with health and/or health care disparities, and how work functions as a social determinant of health. Of particular interest are projects designed to examine pathways and mechanisms using conceptual models grounded in minority health and health disparities theories that recognize that health disparities arise by multiple and overlapping contributing factors acting at multiple levels of influence. Studies must examine NIH-designated U.S. health disparities populations. NIEHS is interested in applications that focus on the intersection of work as a social determinant of health, the physical environment (that includes exposures to toxicants), and other social determinants of health in creating or intensifying environmental health disparities at the population level. Community engaged research approaches are strongly encouraged as well as applications that move the science of environmental health disparities towards achieving environmental justice for affected populations.
Deadline: October 5, 2021; February 5, 2022
Transition to Independent Environmental Health Research Career Award (K01 Independent Basic Experimental Studies with Humans Required)
The Transition to Independent Environmental Health Research career award is a 3-year bridge scholar development program for newly independent faculty who intend to pursue research careers in environmental health sciences. This funding opportunity is designed for applicants proposing to serve as the lead investigator of an independent clinical trial, a clinical trial feasibility study, or a separate ancillary study to an existing trial. For applicants not planning independent basic experimental studies with humans, there are two companion funding opportunities. Applicants planning independent clinical trials with specific application toward processes or with products in mind, must apply to the companion funding opportunity announcement, Transition to Independent Environmental Health Research Career Award (K01 Clinical Trial Required). Applicants not planning an independent clinical trial, or proposing to gain research experience in a clinical trial led by another investigator, must apply to companion funding opportunity announcement, Transition to Independent Environmental Health Research Career Award (K01 Clinical Trial Not Allowed). At the conclusion of the career development period the candidates are expected to demonstrate they can successfully compete for research funding in the environmental health sciences. Eligible candidates for the K01 award must have a research or health-professional doctoral degree and must be within three years of their appointment to their first independent faculty position at the time of submission (receipt date) of the application.
Deadline: October 12, 2021
Research on Autism Spectrum Disorders (R01 Clinical Trial Optional)
This award supports research designed to elucidate the etiology, epidemiology, diagnosis, and optimal means of service delivery in relation to Autism Spectrum Disorders (ASD). The Research Project Grant (R01) mechanism supports discrete, specified projects based in scientific areas that represent the investigators’ specific interests and competencies, and that fall within the mission of the participating NIH Institutes and Centers. Additional companion funding opportunities are available for a Small Research Grant (R03) which supports small, discrete, well-defined projects that can be completed in two years and that require limited resources (Research on Autism Spectrum Disorders (R03 Clinical Trial Optional)); and an Exploratory/Developmental Grant (R21) which encourages exploratory/developmental research by providing support for the early and conceptual stages of project development (Research on Autism Spectrum Disorders (R21 Clinical Trial Optional)). Basic research into the pathophysiology of ASD, including research on brain mechanisms, is of special interest. Also, of high priority are clinical and applied investigations that may lead to the development of new treatments and interventions.
Deadlines: June 16, 2021; October 16, 2021
Maximizing Opportunities for Scientific and Academic Independent Careers (MOSAIC) Postdoctoral Career Transition Award to Promote Diversity (K99/R00 Independent Clinical Trial Not Allowed)
Supports a cohort of early career, independent investigators from diverse backgrounds conducting research in NIH mission areas. The long-term goal of this program is to enhance diversity in the biomedical research workforce. The MOSAIC K99/R00 program is designed to facilitate a timely transition of promising postdoctoral researchers from diverse backgrounds from their mentored, postdoctoral research positions to independent, tenure-track or equivalent research-intensive faculty positions. The MOSAIC K99/R00 program will provide independent NIH research support before and after this transition to help awardees launch successful, independent research careers. This Funding Opportunity Announcement is designed specifically for applicants proposing research that does not involve leading an independent clinical trial, a clinical trial feasibility study, or an ancillary clinical trial. Applicants are permitted to propose research experience in a clinical trial led by a mentor or co-mentor. Applicants proposing a clinical trial or an ancillary clinical trial as lead investigator, should apply to PAR-21-272. Applicants proposing basic science experimental studies involving humans, should apply to PAR-21-273.
Deadline: October 24, 2021
Notice of Special Interest (NOSI): Research Supplements to Promote Re-Entry and Re-integration into Health-Related Research Careers (Admin Supp - Clinical Trial Not Allowed)
Provides support for a mentored research training experience for individuals with high potential to re-enter or re-integrate into an active research career, after an interruption for family responsibilities or other qualifying circumstances. This program encourages re-entry and re-integration administrative supplement applications to existing NIH research grants to support full- or part-time mentored research experiences by these individuals. The supplement grants are intended to provide these scientists an opportunity to update or extend their research skills and knowledge and prepare them to re-establish their careers in basic biomedical, behavioral, clinical, translational, or social science research. Re-entry supplements provide research training opportunities to individuals with doctoral degrees who have had career interruptions of at least six months and no more than eight years. Re-integration supplements allow post-doctoral and predoctoral students the opportunity to transition to a new, safe, and supportive research environment.
Deadlines: November 1, 2021; December 1, 2021
Innovative Approaches for Improving Environmental Health Literacy (R43/R44 Clinical Trial Not Allowed)
Solicits Phase I (R43), Phase II, and Fast-track (R44) Small Business Innovative Research grant applications from small business concerns in collaboration with environmental science researchers to develop novel tools, activities, or materials to build environmental health literacy for a variety of groups, including community members, health care and public health professionals, educators, and students of all ages. See Innovative Approaches for Improving Environmental health Literacy (R41/R42 Clinical Trial Not Allowed) which solicits Phase I (R41), Phase II (R42), and Fast-track (R42) Small Business Technology Transfer grant applications. As part of its Partnerships for Environmental Public Health Program, NIEHS is interested in developing tools that build capacity, improve environmental health literacy, and support citizen science endeavors. In addition, there is a need for improved approaches for communicating Environmental Health Science concepts for diverse audiences, including K-12 education, undergraduate and graduate education, and information for health care professionals. These approaches or resources should be fit-for-purpose to meet the needs of the following audiences: community members, health care and public health professionals, educators, and students of all ages.
Deadline: November 10, 2021
Letter of Intent: October 10, 2021
Mobile Health: Technology and Outcomes in Low and Middle Income Countries (R21/R33 – Clinical Trial Optional)
Encourages exploratory and developmental research applications that propose to study the development, validation, feasibility, and effectiveness of innovative mobile health (mHealth) interventions or tools specifically suited for low- and middle-income countries that utilize new or emerging technology, platforms, systems, or analytics to improve health outcomes. Institutions from both U.S. and low- and middle-income countries are eligible to apply to this funding opportunity, and broad partnerships are strongly encouraged. While it is not required (although it is encouraged) for applications submitted to this announcement by low- and middle-income country institutions; to have U.S. partners, all applications submitted to this announcement by U.S. institutions are required to involve low- and middle-income country researchers as key personnel. Areas of interest to the NIEHS include, but are not limited to: optimizing mHealth technology to prevent or mitigate environmental exposures; development and implementation of mHealth technologies that have the potential to reduce environmental health disparities; using mHealth technology to link to existing datasets to increase access to exposure information and promote health literacy; and using mHealth technology to increase access to resources in low- and middle-income countries to mitigate the effects of climate change and other natural and human caused disasters on human health.
Deadline: November 15, 2021
Letter of Intent: October 16, 2021
NIH Blueprint and BRAIN Initiative Diversity Specialized Predoctoral to Postdoctoral Advancement in Neuroscience Award (F99/K00 Clinical Trial Not Allowed)
The NIH Blueprint and Brain Research through Advancing Innovative Neurotechnologies (BRAIN) Initiative Diversity Specialized Predoctoral to Postdoctoral Advancement in Neuroscience Award is intended for individuals who have demonstrated an interest in a neuroscience research career in NIH Blueprint mission-relevant areas and/or BRAIN Initiative research areas. This award will support a defined pathway across career stages for outstanding graduate students from diverse backgrounds, including those from groups underrepresented in biomedical and behavioral sciences. This two-phase award will facilitate completion of the doctoral dissertation and transition of talented graduate students to strong neuroscience research postdoctoral positions and will provide career development opportunities relevant to their long-term career goal of becoming independent neuroscience researchers.
Deadline: December 15, 2021
Letter of Intent: Due 30 days prior to application due date
PHS 2021-2 Omnibus Solicitation of the NIH, CDC and FDA for Small Business Innovation Research Grant Applications (Parent SBIR [R43/R44] Clinical Trial Not Allowed)
Enables U.S.-owned and operated small businesses to conduct research and development that has a strong potential for commercialization. This award and the associated PHS 2021-2 Omnibus Solicitation of the NIH and CDC for Small Business Innovation Research Grant Applications (Parent SBIR [R43/R44] Clinical Trial Required) provide funds for small businesses to stimulate technological innovation in the private sector and strengthen the role of small business in meeting federal research and development needs. The related Small Business Technology Transfer announcements (PHS 2021-2 Omnibus Solicitation of the NIH for Small Business Technology Transfer Grant Applications (Parent STTR [R41/R42] Clinical Trial Not Allowed) and PHS 2021-2 Omnibus Solicitation of the NIH for Small Business Technology Transfer Grant Applications (Parent STTR [R41/R42] Clinical Trial Required)) aim to foster technology transfer through cooperative research and development between small businesses and research institutions. Applicants are encouraged to submit grant applications in response to NIEHS-identified topics.
Deadline: January 5, 2022
Notice of Intent to Publish a Funding Opportunity Announcement for Virtual Consortium for Translational/Transdisciplinary Environmental Research (ViCTER) (R01 Clinical Trial Optional)
Intent to reissue a funding opportunity announcement for the ViCTER award. The ViCTER program fosters and promotes early-stage transdisciplinary collaborations and/or translational research efforts among fundamental (technology and mechanism oriented), clinical (patient-oriented), and population-based researchers in the environmental health field. This funding opportunity will use the R01 mechanism and will bring together newly established collaborative teams to investigate potential linkages between human health and one or more environmental stressor(s). The ViCTER program is intended to support innovative high-risk, high-reward cross-disciplinary and/or translational research projects that are more difficult to achieve in a typical R01 application. Collaboration among investigators at different institutions through a virtual consortium arrangement are highly encouraged.
Deadline: February 1, 2022









