Public Health Effects of Natural Gas Flaring: Understanding and Communicating Environmental Justice Implications
Unconventional natural oil and gas extraction techniques, such as hydraulic fracturing or “fracking,” have brought oil and gas development activities closer to residential areas. The public health effects of this development are being studied by numerous researchers.
Jill Johnston, Ph.D., studies a specific activity related to oil and gas extraction called flaring, which is the intentional combustion of flammable gases during extraction. Flares can release toxins and contribute to noise and light pollution, but flaring’s impact on public health has not been widely studied until recently.
Johnston and her team found that predominantly Hispanic communities have a disproportionate exposure to gas flaring, and that pregnant Hispanic women exposed to a high number of nightly flares are more likely than non-Hispanic white women to have preterm births and shorter gestational periods.
Health hazards are also associated with other aspects of natural gas extraction. To communicate these public health concerns, Johnston’s team at the University of Southern California (USC) Southern California Environmental Health Sciences Center and community partners of the Trade, Health, Environment Impact Study (T.H.E. Impact Project) recently created an infographic, The Impacts of Natural Gas on Public Health and the Environment. This infographic shares the realities front-line environmental justice communities experience when living near natural gas activities.
“We hope this infographic provides communities with access to key scientific information on the health impacts of natural gas in order to engage in improving environmental health in communities,” said Johnston, assistant professor of preventive medicine at USC.
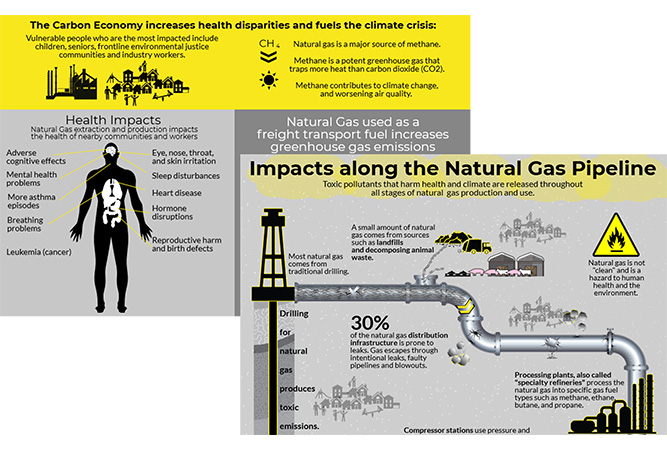
Excerpts of the infographic, The Impacts of Natural Gas on Public Health and the Environment. (Full Infographic) (Photo courtesy of USC Environmental Health Centers)
The Southern California Environmental Health Sciences Center: Committed to Community Engagement and Valuing Community Knowledge
As director of the Southern California Environmental Health Sciences Center’s Community Engagement Core (CEC), Johnston collaborates with community partners to address the effects of the environment on human health. The CEC has developed a model to engage Latinx, Asian/Pacific Islanders, and African Americans living under economic hardship and experiencing health disparities from social and environmental justice issues. The CEC created outreach materials on topics such as near roadway pollution and toxic metals in baby teeth in response to the community’s expressed concerns and questions.
More than 10 CEC community partners helped develop the natural gas infographic. They include the Center for Community Action and Environmental Justice, which works within communities to develop and sustain participatory decision-making that empowers communities, and the East Yard Communities for Environmental Justice.

The community partners that helped develop the natural gas infographic. (Photo courtesy of USC Environmental Health Centers)
Many of the CEC’s resources, including the natural gas infographic, were created in conjunction with the Trade, Health, and Environment Impact Project (T.H.E. Impact Project), a community-academic partnership that combines science, community-based research, and input from affected residents to ensure their perspective is heard. T.H.E. Impact Project trains residents as part of Neighborhood Assessment Teams to gather data on air pollution and report these results to community leaders and elected officials. But T.H.E. Impact Project’s focus is much broader than natural gas development.
“T.H.E. Impact Project was born out of the combined efforts of public health advocates, community residents, and academic and legal partners working together to address the impacts of freight and goods movement on pollution-burdened communities,” said Taylor Thomas, co-Executive Director of East Yard Communities for Environmental Justice. “T.H.E. Impact Project is part of The Moving Forward Network, which is a national network of residents and organizations fighting for clean freight at the federal level. T.H.E. Impact Project has been instrumental in getting clean air policies at our local ports.”
The Environmental Justice Dimensions of Gas Flaring

Are you enjoying the PEPH newsletter? Are there topics you'd like to see discussed more often? Please take a few minutes to provide feedback.
In studying the health effects of oil and gas development on communities, Johnston is also interested in examining the environmental justice aspects of such industrial activities. Two of her recent papers focus on the environmental justice dimensions of gas flaring.
In the paper Environmental Justice Dimensions of Oil and Gas Flaring in South Texas: Disproportionate Exposure among Hispanic Communities, Johnston’s team used satellite observations to identify nightly gas flare events in Texas’ Eagle Ford shale, one of the most productive regions in the U.S. They also used 2010 census data to characterize the demographics of areas near oil and gas extraction activity. Much of the region around the shale is home to families with low incomes, and about 40% of residents identify as Hispanic. The team found that the neighborhoods with a predominantly Hispanic population were exposed to more nightly flares than non-Hispanic white neighborhoods. Examining the data further, the team noticed the predominantly Hispanic communities’ increased exposure to flaring was not due to being closer to more oil wells; therefore, they concluded that the increased exposure to flaring is itself an environmental justice issue.
Johnston’s team also looked at the effects of flaring on birth outcomes in the Eagle Ford shale, as previous research had suggested exposure to oil and gas development can adversely affect birth outcomes. Using administrative birth records and satellite observations of flaring events, the team found that exposure to a high number of nightly flare events increased pregnant women’s chances of having a preterm birth and overall shorter gestational periods. The researchers also found that the relationship between flare events and adverse birth outcomes was true among Hispanic women, but not white women. In light of these findings, Johnston believes flaring may exacerbate existing environmental health disparities.
While Johnston’s papers are about flares in Texas, a better understanding of the health impacts and environmental justice aspects of oil and gas development is more widely applicable, as fracking and flaring have increased nationwide over the last few years.
“This is just the tip of the iceberg in terms of understanding the health effects and environmental justice dimensions of flaring,” said Johnston. “We hope to expand our research to look at communities in west Texas and North Dakota where flaring is rampant and assess impacts on maternal and infant health.”
As Johnston and other researchers learn more about the health effects of oil and gas development, communicating that information to the public will be essential. Therefore, Johnston and the CEC will continue developing tools such as the infographic and the Urban Oil and Gas Production in Los Angeles County story map. She hopes sharing scientific results with the public empowers communities to take action toward improving their environmental health.
Environmental Health Perspectives Journal Creates Wildfire Smoke Curated Collection
The journal Environmental Health Perspectives published the Wildfire Smoke Curated Collection, a compilation of different types of articles that shine a light on wildfire smoke exposures and the resulting health risks.
Wildfires cause immediate danger to those living nearby and to first responders and firefighters, but the unhealthy air quality caused by wildfires also has widespread effects on people living many miles away. Wildfire smoke exposures and the stress of living near a wildfire bring a variety of health impacts, including problems for people with preexisting respiratory conditions, increased risk of hospitalization for cardiopulmonary issues, death, and an elevated risk of adverse birth outcomes.
NIEHS Develops High School Curriculum About COVID-19 and Environmental Determinants of Health
To help high school students learn more about COVID-19, NIEHS developed a curriculum, Examining Risk Factors Associated with COVID-19 Using the Pandemic Vulnerability Index, which highlights COVID-19’s spread and risk factors. The curriculum uses the Pandemic Vulnerability Index (PVI), an epidemiological modeling tool, to allow students to examine COVID-19 vulnerability at the county level. The tool has data for multiple risk factors, such as infection rate, intervention measures, and environmental determinants of health. The curriculum has two lessons: the first focuses on mathematical modeling and using the PVI, while the second probes the relationship between social and environmental determinants of health and COVID-19. The curriculum’s introduction has additional information, including which North Carolina and Common Core educational standards align with the curriculum. NIEHS developed the curriculum as part of its continued educational outreach and community partnership efforts.
Radon as a Women’s Health Issue
January was national radon action month. In this podcast from NIEHS’s Women’s Health Awareness initiative, Phillip Gibson, the North Carolina Radon Program Coordinator for the North Carolina Department of Health and Human Services, discusses radon and the issues surrounding it. He talks about where it is found, the health effects of exposure, and how to protect families against radon exposure.
Public Health Partnership Grantees Pivot to Address COVID-19
The Cross-sector Innovation Initiative (CSII) program is administered through the Public Health National Center for Innovations (PHNCI) and the Center for Sharing Public Health Services (CSPHS), with funding from the Robert Wood Johnson Foundation. It funds multi-sector, community-based partnerships between public health, health care, social service organizations, and communities with the ultimate goal of improving population health, well-being, and equity. The awards range in focus from pregnant mothers and birth outcomes to mental health and social determinants of health.
CSII grantees have developed innovative approaches to address community health needs during COVID-19 pandemic. For example, two local health and human services organizations in Washington shared telehealth consent documentation, combined purchasing power and other resources early in the pandemic. As a result of pooling resources, there was minimal disruption to patient services and administratively, the organizations’ billing configurations were restructured within 72 hours of the state’s stay-at-home order. These types of partnerships are especially important during the COVID-19 pandemic because small, community-based organizations often lack the administrative resources required for swift mobilization and pivoting.

PEPH Environmental Health Chat Podcast Series
NIEHS Program Builds Careers, Changes Lives (Part II)
PEPH Environmental Health Chat Podcast Series
NIEHS Program Builds Careers, Changes Lives (Part II)
In this second podcast about the NIEHS Environmental Career Worker Training Program, hear from Rocio Treminio-Lopez, a program graduate and now mayor of Brentwood, Maryland. She discusses her experience in the program and how it shaped her life and career. The program is celebrating its 25th anniversary.
You can find more podcasts on the Environmental Health Chat webpage or subscribe to the series on iTunes. We want your feedback! Send comments and ideas for future podcasts to [email protected].

PEPH Grantee Highlight
Montgomery Proffit
Montgomery Proffit is passionate about helping people obtain safe and sustainable employment, and he’s dedicated to helping people from disadvantaged communities obtain the skills for work in environmental careers. In 2001, he joined Opportunity Advancement Innovation in Workforce Development (OAI, Inc.), a nonprofit funded by the NIEHS Worker Training Program, as a Welfare to Work case manager. Proffit is now the director of the OAI Environmental Career Working Training Program (OAI ECWTP) Consortium. Proffit says that the people OAI ECWTP serves have experienced social barriers to employment, such as incarceration or addiction, but OAI ECWTP provides support and resources to guide them through these barriers. The program’s success is evident from its 2019 statistics – it trained 85 people, and 80% of them were placed in jobs.
Funding Opportunites
Addressing Health Disparities Among Immigrant Populations Through Effective Interventions (R01 Clinical Trial Optional)
Supports research to design and implement effective interventions to enhance health advantages and reduce the health disparities among U.S. immigrant populations, particularly migrant workers, recent and first-generation immigrants. This announcement calls for multidisciplinary/multilevel research focusing on the design and implementation of effective interventions that will address immigrant-specific factors to reduce health disparities. A framework to demonstrate the multidomain, multilevel factors that may influence health disparities is available here. A life-course perspective is encouraged with interventions focusing attention on transition points across the lifespan and associated risk and protective factors for immigrant populations. Projects should involve collaborations among relevant stakeholders in U.S. immigrant population groups, such as researchers, community organizations, healthcare providers, public health organizations, consumer advocacy groups, and faith-based organizations. Projects must focus on immigrants from one or more NIH-designated populations that experience health disparities in the U.S., which include racial and ethnic minorities (Blacks or African Americans, Hispanics/Latinos, Asian Americans, and Pacific Islanders).
Deadlines: February 5, 2021; June 5, 2021; October 5, 2021
Addressing the Etiology of Health Disparities and Health Advantages Among Immigrant Populations (R01 Clinical Trial Not Allowed)
Supports innovative research to understand factors uniquely associated with the immigration experience that contribute to health disparities or health advantages among U.S. immigrant populations, particularly migrant workers, recent and first-generation immigrants. This announcement calls for multidisciplinary research to address the specific underlying causes and mechanisms of health disparities and health advantages. A framework to demonstrate the multidomain, multilevel factors that may influence health disparities is available here. Projects should involve collaborations among relevant stakeholders in U.S. immigrant population groups, such as researchers, community leaders and organizations, public health organizations, consumer advocacy groups, faith-based organizations, and healthcare providers. Projects must focus on immigrants from one or more NIH-designated populations that experience health disparities in the U.S., which include racial and ethnic minorities (Blacks or African Americans, Hispanics/Latinos, Asian Americans, and Pacific Islanders).
Deadlines: February 5, 2021; June 5, 2021; October 5, 2021
Dissemination and Implementation Research in Health (R01 Clinical Trial Optional)
Supports innovative approaches to identifying, understanding, and developing strategies for overcoming barriers to the adoption, adaptation, integration, scale-up and sustainability of evidence-based interventions, tools, policies, and guidelines. Additionally, there is a benefit in understanding circumstances that create a need to stop or reduce (“de-implement”) the use of interventions that are ineffective, unproven, low-value, or harmful. This FOA invites research grant applications that will identify, develop, test, evaluate, and/or refine strategies to disseminate and implement evidence-based practices (e.g. behavioral interventions; prevention, early detection, diagnostic, treatment and disease management interventions; quality improvement programs) into public health, clinical practice, and community (e.g., workplace, school, place of worship) settings. Studies to advance dissemination and implementation research methods and measures are also encouraged.
Deadlines: February 5, 2021; June 5, 2021; October 5, 2021
Letter of Intent: Due 30 days prior to the application due date
Superfund Hazardous Substance Research and Training Program (P42 Clinical Trial Optional)
Supports problem-based, solution-oriented research Centers that consist of multiple, integrated projects representing both the biomedical and environmental science and engineering disciplines; as well as cores tasked with administrative (which includes research translation), data management and analysis, community engagement, research experience and training coordination, and research support functions. The scope of the Superfund Research Program Centers is taken directly from the Superfund Amendments and Reauthorization Act of 1986, and includes: (1) advanced techniques for the detection, assessment, and evaluation of the effect on human health of hazardous substances; (2) methods to assess the risks to human health presented by hazardous substances; (3) methods and technologies to detect hazardous substances in the environment; and (4) basic biological, chemical, and physical methods to reduce the amount and toxicity of hazardous substances.
Deadline: February 15, 2021
Letter of Intent: January 15, 2021
Outstanding New Environmental Scientist (ONES) Award (R01 Clinical Trial Optional)
Identifies and supports the most talented Early Stage Investigators (ESIs) who intend to make a long-term commitment to research in the Environmental Health Sciences by assisting them in launching an innovative research program focused on understanding the effects of environmental exposure on people’s health. Research projects proposed will be expected to have a defined impact on the environmental health sciences and be responsive to both the mission of the NIH and, specifically, to the mission of the NIEHS and the 2018-2023 Strategic Plan: Advancing Science, Improving Health: A Plan for Environmental Health Sciences Research (7MB). Applicants should consult the Strategic Plan to ensure that the proposed research addresses the goals and priority areas of the NIEHS. This Strategic Plan focuses on discovering how the environment affects people in order to promote healthier lives, conducting and supporting the very best environmental health sciences research in alignment with real-world public health needs, and translating science findings into knowledge that can inform real-life individual and public health outcomes. A variety of scientific disciplines, including basic, mechanistic, clinical, epidemiological, computational, engineering, and/or health risk communication approaches, can be used to advance the Strategic Plan. Only one application per School or College within a University is allowed.
Deadlines: February 26, 2021; February 24, 2022; February 24, 2023
Letter of Intent: Due 30 days prior to the application due date
NIEHS Support for Understanding the Impact of Environmental Exposures on Coronavirus Disease 2019 (COVID-19)
Addresses the urgent need for mission-relevant research to understand the impact of environmental exposures on Coronavirus Disease 2019 (COVID-19) and its causative agent, the virus SARS-Cov-2. NIEHS is particularly interested in applications that will provide insight into the role of environmental exposures in pathogenicity, transmission, individual susceptibility, or prevention and intervention strategies. Examples of environmental exposures relevant to the NIEHS mission include: toxic chemicals, air pollutants, second hand tobacco smoke, e-cigarette vapors, metals, and other environmental chemical exposures that may impact health outcomes. NIEHS is accepting applications addressing COVID-19 through the administrative supplement, urgent competitive revision, and time-sensitive mechanisms.
Deadlines: October 1, 2020; November 2, 2020; December 1, 2020; January 4, 2021; February 1, 2021; March 1, 2021; April 1, 2021; May 3, 2021
Environmental Influences on Aging: Effects of Extreme Weather and Disaster Events on Aging Populations (R01 Clinical Trial Optional)
Supports research to advance our understanding of the impact of extreme weather and disaster events in aging human populations. This FOA (PAR-19-250) and its companion FOA (), which focuses on underlying mechanisms of aging utilizing animal models, will help explicate the behavioral, biological, and socioecological processes that occur during extreme weather or disaster events that affect aging processes. Through the integration of the population studies and the companion mechanistic studies FOA, the goal is to improve the health and well-being of older adults via increased knowledge about extreme weather and disaster preparedness, response, and recovery.
Deadline: July 7, 2020; November 9, 2020; March 8, 2021
Letter of Intent: Due 30 days prior to the application due date
Application of Artificial Intelligence and Machine Learning for Advancing Environmental Health Sciences (R41 Clinical Trial Not Allowed)
Solicits Phase I Small Business Technology Transfer (STTR) grant applications from small business concerns (SBCs) to develop promising methodologies using Artificial Intelligence (AI) and Machine Learning (ML) approaches to advance environmental health research and decisions. When further developed and validated, these methodologies or approaches should improve the accuracy of toxicity prediction, help in prioritizing chemicals for more relevant or targeted testing, identify and/or fill data or knowledge gaps in toxicity assessment, and promote more comprehensive understanding of human exposure effects, susceptibility, and adverse health outcomes.
Deadline: March 29, 2021
Letter of Intent: February 28, 2021
Application of Artificial Intelligence and Machine Learning for Advancing Environmental Health Sciences (R43 Clinical Trial Not Allowed)
Solicits Phase 1 Small Business Innovation Research (SBIR) grant applications from small business concerns (SBCs) to develop promising methodologies using Artificial Intelligence (AI) and Machine Learning (ML) approaches to advance environmental health research and decisions. When further developed and validated, these methodologies or approaches should improve the accuracy of toxicity prediction, help in prioritizing chemicals for more relevant or targeted testing, identify and/or fill data or knowledge gaps in toxicity assessment, and promote more comprehensive understanding of human exposure effects, susceptibility and adverse health outcomes.
Deadline: March 29, 2021
Letter of Intent: February 28, 2021
HEAL Initiative: HEALthy Brain and Child Development Consortium Administrative Core (U24 - Clinical Trial Not Allowed)
Seeking applications for a Consortium Administrative Core for the HEALthy Brain and Child Development (HBCD) Study. This FOA runs in parallel with companion FOAs that seek applications for linked and unlinked research sites and a single Data Coordinating Center. The HBCD Consortium Administrative Core (HCAC) will be responsible for providing the organizational framework for the management, direction, and overall coordination of the national multi-site consortium. It will coordinate the interactions of the individual Research Project Sites and the HBCD Data Coordinating Center. The HCAC will include Administrative and Project Management Plans, and will also be responsible for managing collaborative activities such as the functions of an Expert Scientific Board and oversight of an internal Steering Committee.
Deadline: March 31, 2021
Letter of Intent: March 1, 2021
HEAL Initiative: HEALthy Brain and Child Development Data Coordinating Center (U24 – Clinical Trial Not Allowed)
Seeking applications for a Data Coordinating Center for the HEALthy Brain and Child Development Study. This FOA runs in parallel with companion FOAs that solicit applications for linked and unlinked research sites and a single Consortium Administrative Core. The HBCD Data Coordinating Center (HDCC) will develop the procedures for collection of the core neuroimaging, neuropsychological, and other phenotypic assessment data in a manner that will maximize comparability across the individual research sites of the consortium. The center will perform quality control, data curation, and analysis for the measures collected from the research sites as well as provide data informatics tools for sites and NIH program staff to monitor consortium progress and performance and explore the curated data. The HDCC will facilitate cross-site pooling of data, create a database across assessment modalities, and harmonize with existing large-scale neurodevelopmental research efforts. The HDCC should include a director (or co-directors) and one or more associate directors to ensure that the wide scope of activities are seamlessly coordinated.
Deadline: March 31, 2021
Letter of Intent: March 1, 2021
HEAL Initiative: HEALthy Brain and Child Development Study (Collaborative U01- Clinical Trial Not Allowed)
Seeking applications for linked Research Project Sites for the HEALthy Brain and Child Development (HBCD) Study using the cooperative agreement award mechanism. This FOA runs in parallel with companion FOAs that seek applications for single, unlinked Research Project Sites, a single Consortium Administrative Core, and a single Data Coordinating Center. Seeks applications to create a consortium of research sites in service of the nationwide, multi-site, multi-modal, longitudinal cohort HBCD Study to prospectively examine brain and behavioral development from birth through childhood, including an emphasis on understanding the impact of in utero substance exposure on outcomes. Research sites will enroll pregnant women and collect data from them and their children using methodologies that include neuroimaging, neurophysiology, behavioral and cognitive assessments, and collection of biospecimens.
Deadline: March 31, 2021
Letter of Intent: March 1, 2021
HEAL Initiative: HEALthy Brain and Child Development Study (U01 - Clinical Trial Not Allowed)
Seeking applications for unlinked Research Project Sites for the HEALthy Brain and Child Development (HBCD) Study using the cooperative agreement award mechanism. This FOA runs in parallel with companion FOAs that seek applications for linked Research Project Sites, a single Consortium Administrative Core, and a single Data Coordinating Center. Seeks applications to create a consortium of research sites in service of the nationwide, multi-site, multi-modal, longitudinal cohort HBCD Study to prospectively examine brain and behavioral development from birth through childhood, including an emphasis on understanding the impact of in utero substance exposure on outcomes. Research sites will enroll pregnant women and collect data from them and their children using methodologies that include neuroimaging, neurophysiology, behavioral and cognitive assessments, and collection of biospecimens.
Deadline: March 31, 2021
Letter of Intent: March 1, 2021
KC Donnelly Externship (Admin Supp Clinical Trial Not Allowed)
Supports successful applicants for translational/transdisciplinary opportunities and experiences within other Superfund Research Program (SRP)-funded centers, government laboratories (e.g., US EPA, Agency for Toxic Substances and Disease Registry (ATSDR), NIEHS), or other agencies (state, local, Tribal). To be eligible, an applicant must be a graduate student (Master's or Ph.D.) or a postdoctoral researcher (status must be maintained for duration of externship) conducting research/activities in any SRP R01 grant or project/core within an SRP P42 Center.
Deadline: April 1, 2021
Letter of Intent: Due 30 days prior to the application due date
Intervention Research to Improve Native American Health (R01 Clinical Trial Optional)
Supports research on interventions to improve health in Native American (NA) populations. This includes 1) etiologic research, where there is a significant gap in knowledge, that will directly inform intervention development or adaptations, 2) research that develops, adapts, or tests the efficacy or effectiveness of health promotion and disease prevention interventions, 3) research that tests culturally informed treatment or recovery interventions and 4) where a sufficient body of knowledge on intervention efficacy exists, research on dissemination and implementation that develops and tests strategies to overcome barriers to the adoption, integration, scale-up, and sustainability of effective interventions. Through this initiative, intervention and related research is sought to build upon community knowledge, resources, and resilience to test science-based, culturally appropriate solutions to reduce morbidity and mortality through identification and remediation of precursors to diseases and disorders and through culturally informed treatment.
Deadline: May 17, 2021; May 17, 2022; May 17, 2023
Letter of Intent: Due 30 days prior to the application due date
Immune Development in Early Life (IDEaL) (U01 Clinical Trial Not Allowed)
Supports research to define the mechanisms regulating the establishment, development, and maintenance of immunity throughout childhood, including the impact of pathogenic or commensal microbes or vaccination against infectious diseases, allergens, or environmental pollutants on immune ontogeny and function. This program will establish collaborations among immunologists, neonatologists, pediatricians, systems biologists, and microbiologists to expand our knowledge of the developing immune system. Knowledge obtained through this program may be applied to the design of improved vaccines and immunotherapies to combat infections or treat/prevent immune-mediated diseases in this vulnerable population.
Deadline: June 4, 2021
Letter of Intent: Due 30 days prior to the application due date
Immune Development in Early Life (IDEaL) (U19 Clinical Trial Not Allowed)
Supports research to define the mechanisms regulating the establishment, development, and maintenance of immunity throughout childhood, including the impact of pathogenic or commensal microbes or vaccination against infectious diseases, allergens, and environmental pollutants on immune ontogeny and function. This program will establish collaborations among immunologists, neonatologists, pediatricians, systems biologists, and microbiologists to expand our knowledge of the developing immune system. Knowledge obtained through this program may be applied to the design of improved vaccines and immunotherapies to combat infections or treat/prevent immune-mediated diseases in this vulnerable population.
Deadline: June 4, 2021
Letter of Intent: Due 30 days prior to the application due date
Native American Research Centers for Health (S06 Clinical Trials Optional)
Invites applications from federally recognized Tribes and Tribal organizations for the Native American Research Centers for Health (NARCH) initiative, which supports biomedical research and career enhancement opportunities to meet health needs prioritized by American Indian or Alaska Native communities. The NARCH initiative also supports research capacity building and the development of research infrastructure to enhance the biomedical research capabilities of these communities.
Deadline: July 24, 2020; June 24, 2021
Letter of Intent: Due 30 days prior to the application due date
NIH Countermeasures Against Chemical Threats (CounterACT) Research Centers of Excellence (U54 Clinical Trial Optional)
The mission of the NIH CounterACT program is to foster and support research and development of new and improved therapeutics for chemical threats. Chemical threats are toxic chemicals that could be used in a terrorist attack or accidentally released from industrial production, storage or shipping. They include traditional chemical warfare agents, toxic industrial chemicals, pharmaceutical-based agents, and pesticides. The Centers will contain at least three research projects supported by an administrative core, up to three optional scientific cores, a research education core, and a pilot project program to support short-term innovative research and recruitment of new investigators into the field of medical countermeasures research. Each research project must include milestones that create discrete go or no-go decision points in a progressive translational study plan.
Deadlines: September 14, 2021; September 13, 2022; September 12, 2023
Letter of Intent: Due 30 days prior to the application due date









